Intraoral scanners In dentistry – an update on digital technology
With the introduction of the first intraoral scanner, CEREC (Chairside Economical Restoration of Esthetic Ceramics) by Dentsply Sirona in 1985, dentistry was offered an exciting alternative to conventional means of impression-taking. Since then, digital technology has developed, resulting in faster, more accurate and smaller scanners than ever before.
As of writing, approximately 15 separate intraoral scanners are available from a variety of companies – all competing within a fierce, growing market. In 2014, the global intraoral scanner market was valued at US$55.3 million, estimated to expand with an annual growth rate of 13.9 per cent from 2015 to 2022 1.
Intraoral scanners have gained traction within the orthodontic speciality, with restorative dentistry following suit. Intraoral scanning technology aims to address fundamentally multiple contemporary clinical issues, including the intuitively error-prone volumetric changes of impression materials and the expansion of dental stone.
This review will provide an overview of the advantages, limitations and clinical applicability of intraoral scanners and serve as an introduction for those unfamiliar with this technology.
Firstly, it is pertinent to discuss the technology of intraoral scanners. The objective of an intraoral scanner is to record precisely the 3D geometry of an object, to allow this to be subsequently used to produce customised dental devices. The fundamentals of intraoral scanning relate to structured light being cast upon an object to be scanned by a handheld device. Images of the object of interest are then captured by image sensors within the handheld scanner and processed by software. This results in the production of a point cloud which is further analysed by software to create a 3D surface model, also known as a mesh 2. The most widely used output file is the STL (stereolithography/standard tessellation language 3).
Numerous technologies exist to process scan data including: triangulation, confocal, active wavefront sampling (AWS) and stereophotogrammetry.
Triangulation works by the concept that the point of a triangle (object of interest) can be calculated knowing the positions and angles of images from two points of view.
Confocal technology relates to the acquisition of focused and defocused images from selected depths – the sharpness of the image infers distance between points and is related to the focal length of the lens 4.
AWS needs a camera and an off-axis aperture module. The module moves around a circular path centred on a point of interest – the distance and depth information are derived from a pattern produced by each point5.
Stereophotogrammetry estimates all co-ordinates through analysing images using an algorithm – relying on passive light projection and software as opposed to active light projection and expensive hardware.
| Advantages | Limitations |
|---|---|
| Enhanced patient comfort | Initial learning curve |
| Gag reflex management | Unable to displace soft tissue – marginal inaccuracies |
| No physical study models requiring storage | Expensive hardware/annual software agreement |
| Streamlined workflow | Unpredictable for extended edentulous sites |
| Predictable for single teeth/implants/short span bridgework (<5 units) | Unable to register dynamic soft tissue relationships |
| Immediate preperation feedback in high magnification (undercut/margin depths) | Requires laboratory familiar with digital technology |
| Improved patient communication |
No matter the imaging processing technology, this data is then constructed into a virtual 3D model. The major challenge of this is rendering a point of interest taken at multiple angles. Accelerometers within the handheld scanner allow distances and angles to be measured between images, with extreme points eliminated statistically, culminating in the production of an STL file suitable for further use to create the custom dental device6.
The accuracy of an intraoral scan is paramount for a well-fitting custom dental prosthetic. This is assessed through the values of “trueness” – being the measured deviation from the actual value and “precision” – the repeatability of multiple measurements.
These terms were defined by the International Organization for Standardization – standard 5725-1. Studies investigating the accuracy of intraoral scanners should ideally include both measurements, to adequately represent both how “correct” a scanner is, as well as how predictably similar its measurements are.
In 2016 8, Ender and co-workers, and other studies, demonstrated intraoral scanner trueness of between 20 m and 48µm and precision between 4µm and 16µm 9-11.
Later, in 2017, Imburgia et al 7 reported scanner trueness and precision in the region of 45µm and 20µm respectively for the most accurate scanners tested. To put these figures into perspective, conventional impression trueness and precision is generally reported in the region of 20µm and 13µm respectively12-14. In its totality, the literature currently reports intraoral scanning is at least as accurate as conventional methods of impression-taking, subject to the complexity of the clinical case 11,15,16.
A common finding is that of partial scans being the most reliable and accurate, when compared to full arch scans2,17,18. When scanning over five units (implants or teeth), the data would suggest scanning is not as predictable as conventional impressions7.
Full arch scans are shown to suffer distortion, specifically at the distal end of the scan 17, 19, 20. Therefore, the scanning of extended preparations or the edentulous mandible is at high risk of error. Shorter scan distances therefore yield the most accurate results9, 21. A clinically acceptable marginal gap for an indirect restoration may be defined at below 100µm22-25.
It is evident that intraoral scanners can achieve errors of consistently less than this value (in single tooth and limited span situations), giving clinical validity.
Advantages
Intraoral scanning provides many advantages for the clinician within single unit, tooth or implant supported restoration or full arch appliance (such as orthodontic retainers or aligners 26-28) situations. Digital records of the patient obviate the need to store plaster models. This has positive implications for storage and consumable costs 27. This data also allows the clinician to easily and accurately monitor changes within the dentition over time – for example, tooth wear or orthodontic relapse 5. It has been evidenced by multiple authors7, 11, 27, 29. that intraoral scanning results in less patient discomfort compared to conventional impressions.
Patients also prefer scanning to conventional methods of impression-taking 28,30 and gag reflexes can be avoided. There is a modest improvement in chairside time 30,31 with a reported average scan time of between four and 15 minutes4, however, greater time saving is gained through the elimination of certain following laboratory steps. A small quadrant scan is ideal for a single restoration 9,32.
Scans of prepared teeth can be scrutinised by the clinician at extreme magnification and software overlays of undercuts/preparation depths are available, with potential for improved clinical outcomes as a result. Files can be directly emailed to the laboratory – thus avoiding the need to physically post an impression. The dental technician can also assess the impression in real time and request another scan to be taken – avoiding an extra visit for the patient 33,34.
Certain problematic sections can be retaken thus avoiding the need to retake a full impression. Patients are shown to feel more involved with treatment and are interested in scanning technology – serving as a good advertising tool35-37.
Limitations
Limitations exist within the practice of intraoral scanning however. As previously mentioned, scanning is currently predictable only within limited parameters. Full arch implant retained prostheses, extended bridgework and complete dentures are currently not supported by compelling evidence. In relation to complete dentures, a predictable dynamic impression of soft tissue borders, muscle attachments and mucosal compressibility is currently severely limited by technology 2.
There is an accepted learning curve in relation to intraoral scanning. It has been reported that subjects with a greater affinity for the world of technology will find the technology easier to adopt than those without this affinity 36,38,39. Issues arise in the detection of deep margins of prepared teeth39 as light cannot record the ‘non visible’ areas of the preparation 2 as normally conventional impression material may be able to displace the gingival margin and record valuable data, following the retraction process. As with conventional impressions, blood or saliva may obscure important margins 40.
With good technique and speed, it has been reported one can overcome many of the reported limitations15,29. The issue of reflective restorations or teeth may also arise. This can result in disruption of the matching of points of interest within the software – resulting in an inaccurate 3D model. This can be counteracted by changing the orientation of the scanner to increase diffuse light, using a camera with a polarizing filter or coating the teeth in powder. Powder coatings (aluminium oxide) can add a variable thickness of up to 90µm41 and further issues arise if taking a full arch scan as powder inevitably gets mixed with saliva – resulting in time spent cleaning teeth and reapplying powder 29.
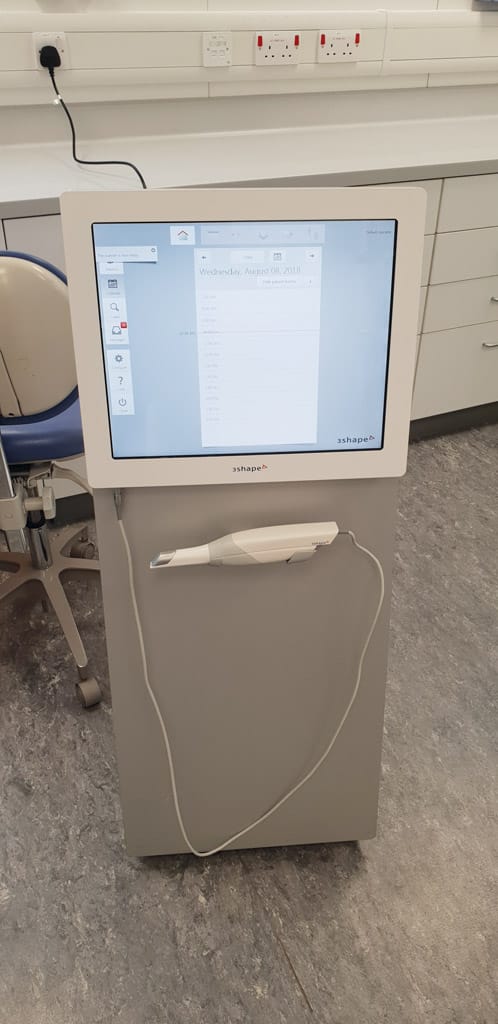
- Figure 1: Mid scan
- Figure 2: Three-shape unit
- Figure 3: Scan of quadrant shown in clinical photo
The scan path can also affect the quality of the scan42 and can result in lost tracking. This should ideally be at a constant distance from the point of interest and moved in a fluid manner, avoiding jerky or fast movements – this can be clinically challenging6. When scanning and tracking is lost, one should return to an area easily recognisable by the software – for example, the occlusal surface of a molar – to predictably re-establish tracking. If scanning a complete arch, multiple small interocclusal records appear to be the most predictable method of achieving accurate articulation or a small scan of the anterior sextants, as described by a 2018 study 32.
The initial expense and management costs of hardware may also be prohibitive – the average intraoral scanner costs between £13,000 and £31,000. An annual update agreement may also exist to “unlock” STL files for use of the laboratory – this again has an associated cost.
As more scanners reach the market, it is likely these costs will become more competitive and attractive to new adopters.
Conclusion
In conclusion, intraoral scanning presents a viable alternative to (and occasionally outperforms) conventional impression techniques within the confines of strict case criteria. Despite being in its late “innovator” and “early adopter phase”, intraoral scanning has shown great potential within restorative dentistry, orthodontics and more recently guided implant surgery (combined with CBCT) 43. Many of its limitations can be circumvented with good clinical technique. Technology, potentially prohibitive costs and market inertia currently prevent its routine use in a wide array of clinical situations.
Author
M Paterson, Specialty Registrar in Restorative Dentistry/Honorary Clinical Lecturer,
Glasgow Dental Hospital & School
References
- ltd RaM. Global Standalone Intraoral Scanners Market Size, Market Share, Application Analysis, Regional Outlook, Growth Trends, Key Players, Competitive Strategies and Forecasts, 2015 to 2022. 2018.
- Mangano F, Gandolfi A, Luongo G, Logozzo S. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health. 2017;17(1):149.
- Treesh JC, Liacouras PC, Taft RM, Brooks DI, Raiciulescu S, Ellert DO, et al. Complete-arch accuracy of intraoral scanners. J Prosthet Dent. 2018.
- Emilia Taneva BKaCAE. Issues in Contemporary Orthodontics. 2015.
- Logozzo S, Zanetti EM, Franceschini G, Kilpelä A, Mäkynen A. Recent advances in dental optics – Part I: 3D intraoral scanners for restorative dentistry. Optics and Lasers in Engineering. 2014;54:203-21.
- Richert R, Goujat A, Venet L, Viguie G, Viennot S, Robinson P, et al. Intraoral Scanner Technologies: A Review to Make a Successful Impression. J Healthc Eng. 2017;2017:8427595.
- Imburgia M, Logozzo S, Hauschild U, Veronesi G, Mangano C, Mangano FG. Accuracy of four intraoral scanners in oral implantology: a comparative in vitro study. BMC Oral Health. 172017.
- Ender A, Zimmermann M, Attin T, Mehl A. In vivo precision of conventional and digital methods for obtaining quadrant dental impressions. Clin Oral Investig. 2016;20(7):1495-504.
- Vecsei B, Joos-Kovacs G, Borbely J, Hermann P. Comparison of the accuracy of direct and indirect three-dimensional digitizing processes for CAD/CAM systems – An in vitro study. J Prosthodont Res. 2017;61(2):177-84.
- Jacob HB, Wyatt GD, Buschang PH. Reliability and validity of intraoral and extraoral scanners. Prog Orthod. 162015.
- Ahlholm P, Sipila K, Vallittu P, Jakonen M, Kotiranta U. Digital Versus Conventional Impressions in Fixed Prosthodontics: A Review. J Prosthodont. 2018;27(1):35-41.
- Ender A, Mehl A. Accuracy of complete-arch dental impressions: a new method of measuring trueness and precision. J Prosthet Dent. 2013;109(2):121-8.
- Seelbach P, Brueckel C, Wostmann B. Accuracy of digital and conventional impression techniques and workflow. Clin Oral Investig. 2013;17(7):1759-64.
- Anadioti E, Aquilino SA, Gratton DG, Holloway JA, Denry I, Thomas GW, et al. 3D and 2D marginal fit of pressed and CAD/CAM lithium disilicate crowns made from digital and conventional impressions. J Prosthodont. 2014;23(8):610-7.
- Ting-Shu S, Jian S. Intraoral Digital Impression Technique: A Review. J Prosthodont. 2015;24(4):313-21.
- Rutkunas V, Geciauskaite A, Jegelevicius D, Vaitiekunas M. Accuracy of digital implant impressions with intraoral scanners. A systematic review. Eur J Oral Implantol. 2017;10 Suppl 1:101-20.
- Patzelt SB, Emmanouilidi A, Stampf S, Strub JR, Att W. Accuracy of full-arch scans using intraoral scanners. Clin Oral Investig. 2014;18(6):1687-94.
- Hack G. Digital Impressions – Clinical Applications of Digital Dental Technology – Wiley Online Library. 2015.
- Gan N, Xiong Y, Jiao T. Accuracy of Intraoral Digital Impressions for Whole Upper Jaws, Including Full Dentitions and Palatal Soft Tissues. PLoS One. 112016.
- Ender A, Attin T, Mehl A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J Prosthet Dent. 2016;115(3):313-20.
- Guth JF, Runkel C, Beuer F, Stimmelmayr M, Edelhoff D, Keul C. Accuracy of five intraoral scanners compared to indirect digitalization. Clin Oral Investig. 2017;21(5):1445-55.
- Bjorn AL, Bjorn H, Grkovic B. Marginal fit of restorations and its relation to periodontal bone level. II. Crowns. Odontol Revy. 1970;21(3):337-46.
- Martinez-Rus F, Suarez MJ, Rivera B, Pradies G. Evaluation of the absolute marginal discrepancy of zirconia-based ceramic copings. J Prosthet Dent. 2011;105(2):108-14.
- McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971;131(3):107-11.
- Renne W, McGill ST, Forshee KV, DeFee MR, Mennito AS. Predicting marginal fit of CAD/CAM crowns based on the presence or absence of common preparation errors. J Prosthet Dent. 2012;108(5):310-5.
- Aragon ML, Pontes LF, Bichara LM, Flores-Mir C, Normando D. Validity and reliability of intraoral scanners compared to conventional gypsum models measurements: a systematic review. Eur J Orthod. 2016;38(4):429-34.
- Goracci C, Franchi L, Vichi A, Ferrari M. Accuracy, reliability, and efficiency of intraoral scanners for full-arch impressions: a systematic review of the clinical evidence. Eur J Orthod. 2016;38(4):422-8.
- Christensen GJ. The Challenge to Conventional Impressions. The Journal of the American Dental Association. 2008;139(3):347-9.
- Zimmermann M, Mehl A, Mormann WH, Reich S. Intraoral scanning systems – a current overview. Int J Comput Dent. 2015;18(2):101-29.
- Yuzbasioglu E, Kurt H, Turunc R, Bilir H. Comparison of digital and conventional impression techniques: evaluation of patients’ perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health. 2014;14(1):10.
- Gjelvold B, Chrcanovic BR, Korduner EK, Collin-Bagewitz I, Kisch J. Intraoral Digital Impression Technique Compared to Conventional Impression Technique. A Randomized Clinical Trial. J Prosthodont. 2016;25(4):282-7.
- Edher F, Hannam AG, Tobias DL, Wyatt CCL. The accuracy of virtual interocclusal registration during intraoral scanning. J Prosthet Dent. 2018.
- Schepke U, Meijer HJ, Kerdijk W, Cune MS. Digital versus analog complete-arch impressions for single-unit premolar implant crowns: Operating time and patient preference. J Prosthet Dent. 2015;114(3):403-6.e1.
- Joda T, Bragger U. Digital vs. conventional implant prosthetic workflows: a cost/time analysis. Clin Oral Implants Res. 2015;26(12):1430-5.
- Lecocq G. Digital impression-taking: Fundamentals and benefits in orthodontics. Int Orthod. 2016;14(2):184-94.
- Kim J, Park JM, Kim M, Heo SJ, Shin IH. Comparison of experience curves between two 3-dimensional intraoral scanners. J Prosthet Dent. 2016;116(2):221-30.Lee SJ, Gallucci GO. Digital vs. conventional implant impressions: efficiency outcomes. Clin Oral Implants Res. 2013;24(1):111-5.
- Marti AM, Harris BT, Metz MJ, Morton D, Scarfe WC, Metz CJ, et al. Comparison of digital scanning and polyvinyl siloxane impression techniques by dental students: instructional efficiency and attitudes towards technology. Eur J Dent Educ. 2017;21(3):200-5.
- Lim JH, Park JM, Kim M, Heo SJ, Myung JY. Comparison of digital intraoral scanner reproducibility and image trueness considering repetitive experience. J Prosthet Dent. 2018;119(2):225-32.
- Aubreton. Infrared system for 3D scanning of metallic surfaces | SpringerLink. 2013.
- da Costa JB, Pelogia F, Hagedorn B, Ferracane JL. Evaluation of different methods of optical impression making on the marginal gap of onlays created with CEREC 3D. Oper Dent. 2010;35(3):324-9.
- Muller P, Ender A, Joda T, Katsoulis J. Impact of digital intraoral scan strategies on the impression accuracy using the TRIOS Pod scanner. Quintessence Int. 2016;47(4):343-9.
- De Vico G, Ferraris F, Arcuri L, Guzzo F, Spinelli D. A novel workflow for computer guided implant surgery matching digital dental casts and CBCT scan. Oral Implantol (Rome). 92016. p. 33-48.




Comments are closed here.