Crown-to-implant ratio
Marginal bone stability around extra-short implants supporting a fixed partial prosthesis in posterior mandible
Short and extra-short implants are a powerful tool in oral implantology these days 1. The use of these implants facilitates the rehabilitation of very resorbed edentulous ridges with a simple approach. The principal problem with the short implants, and most commonly with extra-short implants, is the crown-to-implant (CI) ratio. The high space to rehabilitate and the longitude of these implants creates an unfavourable prosthesis on the basis of the CI ratio.
The CI ratio is a term imported by the general odontology, and the use of these parameters in implants is used in a similar way. The use of the concept in general odontology translates to the use of implant prosthesis, and while they have similar points they also have some big differences. The most important difference is the biomechanical behaviour of the implant-prosthesis conjunct and the way to convey the stress to the crestal bone. The absence of periodontal ligament and the anchylotic union between the bone and the implant may generate a great force in the crestal bone and we can think how this increase produces a major bone resorption.
In relation to these differences between the length of the restorations and implants it would appear to indicate a bad biomechanical behaviour of the assembly with impact on the marginal bone loss and increasing the rate of failure. To analyse the studies published in relation to this topic, they do not show how a greater bone loss in high crown-implant ratios and ratios higher than two has been considered a safe and predictable therapeutic option 2–5.
To assess the outcomes, implants were followed clinically and radiographically to identify crestal bone loss and implant failure
The aim of this study was to evaluate the effect of the CI ratio on the marginal bone stability around extra-short implants supporting a fixed-partial prosthesis in posterior mandible. The secondary outcome was to the
implant survival.
Material and methods
This manuscript was written according to the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines 6. All described data and treatments were obtained from a single dental clinic in Vitoria, Spain. Patients’ records were retrospectively reviewed to identify patients that fulfilled the following inclusion criteria:
Aged over 18 years old
Placement of extra-short (length ≤ 6.5 mm) implants before December, 2010
Placed in posterior mandible.
The principal outcome was the marginal bone loss and the secondary outcome was the implant survival rate.
Patients or implants that did not meet any of these criteria were excluded from the study. Prior to surgery, and in order to make a proper treatment plan, all patients underwent standard diagnostic protocol consisting of reviewing the medical and dental history, diagnostic casts, and radiographic evaluation.
To assess the principal and secondary outcomes, implants were followed clinically and radiographically to identify the crestal bone loss and implant failure (failure to achieve osseointegration or loss of acquired osseointegration).
The measurement of the marginal bone loss was performed on the most recent radiograph. To do that, known implant length was used to calibrate the linear measurements on the radiograph. Then, the distance between the uppermost point of the implant platform and the most coronal bone-implant contact was measured mesial and distal to the implant by computer software (Sidexis, Sirona, USA). The bone level recorded just after the placement of the provisional prosthesis served as a reference for the measurement of the marginal bone loss. The bone loss was measured mesially and distally to the implant. Finally, a mean of the two measurements were reported due to the absence of statistically
significant differences.
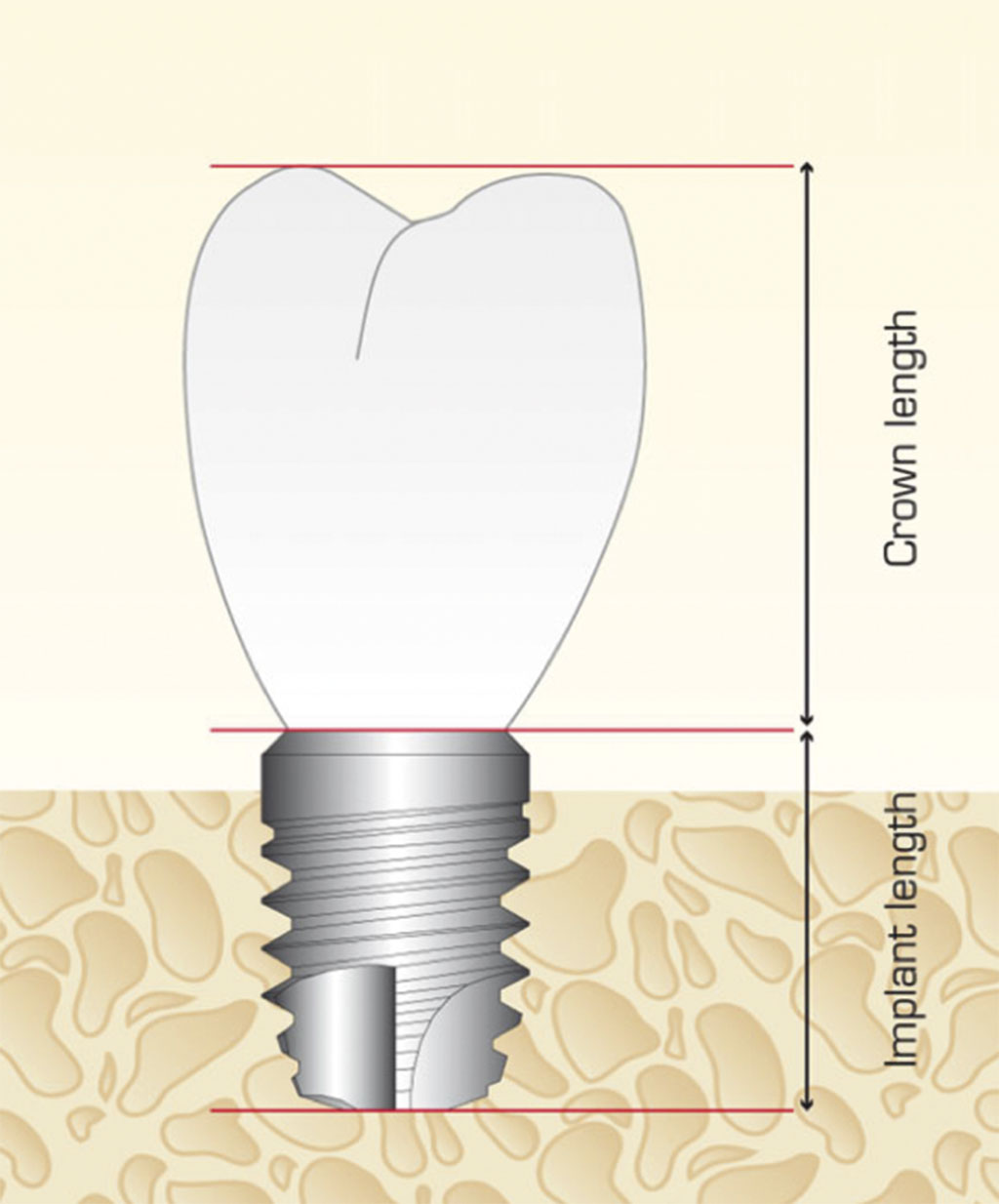
The crown-implant ratio was determined by two measurements: the crown was measured from the tip of the highest cusp to the platform of the implant, along a perpendicular line. The implant was then measured at the centre, from the platform to the end of the apex (Figure 1).
In all patients, the same surgical protocol was followed. Before surgery, patients underwent a routine dental scaling to start the implant treatment with adequate periodontal health. Radiographic evaluation was also performed to establish the treatment plan. All patients received prophylactic antibiotic medication before and after surgery. An infiltrative anaesthesia was applied and incisions were made to elevate a full-
thickness flap.
Implant sites were prepared using a low-speed drilling procedure (125 rpm) without irrigation 7,8. Before installation, implants were carefully embedded in liquid Plasma Rich in Growth Factors (PRGF) prepared from patient’s blood according to a protocol developed by the manufacturer (PRGF-Endoret, Biotechnology Institute BTI, Vitoria, Spain) to bioactivate the implant surface.
For placing the dental implant, the surgical motor was set at 25 Ncm and the implants were finally seated manually by a calibrated torque wrench. The final insertion torque was annotated in the patient’s record.
A prosthodontist performed the prosthetic rehabilitation of the patients. Impression copings were placed and an impression was made with polyether impression material (Impregum Penta; 3M ESPE) and the open-tray technique at three months after implant insertion.
The follow-up visits were scheduled for a series of periodic evaluations, consisting normally of visits at one week after intervention, at one month, at three months, at six months, and from this moment ahead, once a year.
- Figure 2. Location, diameter and length of the implants included in the study
- Figure 3a. Intraoral pictures of the patient. In these images we can see the partial edentulism in mandible and total edentulism in the maxillae. A) front view B) lateral view
- Figure 3b. Intraoral pictures of the patient. In these images we can see the partial edentulism in mandible and total edentulism in the maxillae. A) front view B) lateral view
- Figure 4. Initial panoramic X-Ray
- Figure 5. Planification of dental implants in the cone-beam with the software BTI-Scan III
- Figure 6. Image of the implant surgery where we can see the insertion of an implant extra-short in the most distal area of the fourth quadrant. The extreme bone resorption at this level requires the implementation of a technique of vertical growth
- Figure 7. Post-operative Rx. In the area of the extra-short implant we can see the bone volume used for the vertical growth
- Figure 8. Panoramic X-Ray at one year follow-up post loading. In the fourth quadrant we can observe the crown-implant ratio of the extra-short implant
- FIGURE 9 X-ray of the follow-up to seven years. We can see the stability of the bone at crestal level
Statistical analysis
Data collection and analysis was performed by two independent examiners. The patient was the statistical unit for the statistical description of demographic data, social habits and medical history. The implant served as the statistical unit for the descriptions of implant length, diameter, location, insertion torque, marginal bone loss and survival of the implants. Absolute and relative frequency distributions were calculated for qualitative variables and mean values and standard deviations for quantitative variables. The Shapiro-Wilk test was selected to check the normal distribution of the data.
The cumulative survival rate of implants were analysed using a life-table analysis (Actuarial method). SPSS v15.0 for Windows statistical software package (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Results
In this study, 32 patients participated with 46 implants with a Crown-implant ratio higher than 1. The patients’ mean age was 68 ± six years (range: 55 to 74 years) at the time of surgery and 78.3 per cent of the patients were females.
Three patients were smokers (4.8 per cent), and none of them referred alcohol habits. One of the patients was diabetic (1.6 per cent), seven patients had previous periodontal disease (11.1 per cent), one patient had previous radiation (1.6 per cent).
The diameter, length and position of the implants included in the study are shown in Figure two. The mean of the follow-up was 23 ± eight months (range 14 to 43). The mean crown-implant ratio was 2.4 ± 0.47 (range 1.50-3.64).
Regarding the type of prosthesis, all patients were rehabilitated using fixed-partial prosthesis. In total, 67.4 per cent of the restorations were screw-retained prosthesis and the rest were cemented.
The measurement of marginal bone loss (MBL) was performed at 12 and 24 months of loading. The mean of mesial bone loss was 1.04 ±0.70 mm and the mean distal bone loss was 0.94 ± 0.71 mm. There was no statistically significant difference between the MBL measurements at different follow-up times (p > .05), indicating that bone level around implants under functional loading was stable over time. No significant influence was found between the CI ratio and MBL, even considering separately CI < 2 and CI ≥ 2.
The overall survival rates of short implants and prosthesis were 100 per cent for the implant and patient-based analysis, respectively, at the end of the follow-up time. In figures three to 10 we show a case of the patients included in the study.
Discussion
The prosthetic rehabilitations in which short implants are involved often lead to imbalances between the lengths of the crowns and the implants. It has been suggested that disproportionate prosthetic restorations could induce poor biomechanical behaviour with a potential impact on MBL and reduced implaent survival rate 9. In this study, no associations between CI ratio of implant-supported prostheses in extra-short implants and MBL were found. Previous studies in which short implants were used have evaluated the influence of CI ratio on marginal bone loss (MBL) 10–12. In general, most of these studies concluded that no relation may be established between an unfavourable CI ratio and MBL, independently of the type of prosthetic rehabilitation 10–12.
All the implants included in this study were splinted restorations. Short and extra-short implants have shown better biomechanical behaviour when the prosthesis have been splinted. An additional rationale for splinting implant crowns together is to favourably distribute the non-axial loads, minimising their transfer to the restoration and supporting bone, and increasing the total load area 13,14. Splinting the crowns reduced the peri-implant bone stress under horizontal load in a finite element analysis model especially recommended for implants surrounded by poor-quality bone 13,15.
When placing extra-short implants, it is necessary to carry out adequate planning and the splinting implants are a correct protocol in these cases 16,17.
Conclusions
Within the limitations of this study, the results show that an increased crown-to-implant ratio in extra-short implants has no significant influence on crestal bone loss and implant survival. The limitations of this study include its retrospective design, the small sample size and short follow-up time. Further studies with more extra-short implants followed for a longer period of time are necessary to establish sound conclusions about the effect of increased crown-to-implant ratio on implant survival.
About the author
Eduardo Anitua DDS, MD, PhD graduated with a degree in medicine and surgery from the University of Salamanca and gained his PhD in medicine from the University of Valencia. He holds a specialism in stomatology from the University of the Basque Country (UPV/EHU) and a diploma in prostheses and occlusion from the Pankey Institute (Florida, USA). He is a visiting professor at more than 20 universities in the USA (Harvard, Boston, Tufts, Pennsylvania, New Orleans), Germany (Berlin), England (Bristol), Italy (Milan, Turin), India, Mexico, Brazil, Portugal, Argentina, Colombia, Venezuela, Uruguay and Spain (Seville, Madrid, Barcelona, Murcia). Dr Anitua has published more than 200 papers in national and international journals, is the author of eight books and co-author of seven books and chapters translated into various languages. He has 37 international patents developed in regenerative therapy and oral implantology.
References
1. Gonçalves TM, Bortolini S, Martinolli M, Alfenas BF, Peruzzo DC, Natali A, Berzaghi A, Garcia RC. Long-term Short Implants Performance: Systematic Review and Meta-Analysis of the Essential Assessment Parameters. Braz Dent J. 2015;26:325-36.
2. Rokni S, Todescan R, Warson P, Pharoah M, Adegbembo AO, Deporter D. An assessment of crown-to-root ratios with short sintered porous-surfaced Implants supporting prostheses in partially edentulous patients. INT J ORAL MAXILLOFAC IMPLANTS 2005;20:69–76
3. Blanes RJ, Bernard JP, Blanes ZM, Belser UC. A 10-year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin. Oral Impl. Res. 18, 2007; 707–714
4. Schneider D, Witt L, Ha ̈mmerle CHF. Influence of the crown-to-implant length ratio on the clinical performance of implants supporting single crown restorations: a cross- sectional retrospective 5-year investigation. Clin. Oral Impl. Res. 23, 2012;169–174.
5. Sanz M, Naert I; Working Group 2. Biomechanics/risk management (Working Group 2). Clin Oral Implants Res. 2009;20(suppl 4):107-111.
6. Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453-1457.
7. Anitua E, Alkhraisat MH, Pinas L, Orive G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann Anat.
8. Anitua E, Carda C, Andia I. A novel drilling procedure and subsequent bone autograft preparation: a technical note. Int J Oral Maxillofac Implants 2007; 22: 138-145.
9. Blanes RJ, Bernard JP, Blanes ZM, Belser UC. A 10-year prospective study of ITI dental implants placed in the pos- terior region. II: influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin Oral Implants Res 2007; 18:707–714.
10. Rokni S, Todescan R, Watson P, Pharoah M, Adegbembo AO, Deporter D. An assessment of crown-to- root ratios with short sintered porous-surfaced implants supporting prostheses in partially edentulous patients. Int J Oral Maxillofac Implants 2005; 20:69–76.
11. Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants 2006; 21:275–282.
12. Birdi H, Schulte J, Kovacs A, Weed M, Chuang SK. Crown- to-implant ratios of short-length implants. J Oral Implantol 2010; 36:425–433.
13. Nissan J, Ghelfan O, Gross O, Priel I, Gross M, Chaushu G. The effect of crown/implant ratio and crown height space on stress distribution in unsplinted implant supporting restorations. J Oral Maxillofac Surg 69:1934-1939, 2011
14. Nissan J, Ghelfan O, Gross O, Priel I, Gross M, Chaushu G. The effect of splinting implant-supported restorations on stress distribution of different crown-implant ratios and crown height spaces. J Oral Maxillofac Surg 69:2990-2994, 2011
15. Grossmann Y, Finger IM, and Block MS. Indications for Splinting Implant Restorations. J Oral Maxillofac Surg 2005; 63:1642-1652.
16. Anitua E, Piñas L, Orive G. Retrospective study of short and extra-short implants placed in posterior regions: influence of crown-to-implant ratio on marginal bone loss. Clin Implant Dent Relat Res. 2015;17:102-10.
17. Anitua E, Alkhraist MH, Piñas L, Begoña L, Orive G. Implant survival and crestal bone loss around extra-short implants supporting a fixed denture: the effect of crown height space, crown-to-implant ratio, and offset placement of the prosthesis. Int J Oral Maxillofac Implants. 2014;29:682-9.
Verifiable CPD Questions
Aims and Objectives:
Assess the marginal bone stability around extra-short implants
Assess the influence of increased crown-to-implant ratio on the marginal bone loss
Assess the survival of extra-short implants placed in atrophic alveolar ridge.
LEARNING OUTCOMES:
Surgical alternatives in the treatment of atrophic alveolar ridge
Definition of the implant crown-to-
implant ratio
Predictability of extra-short implants to support a fixed prosthesis.
example question:
To measure the crown-to-implant ratio, the following measurements are needed:
A. The crown length
B. The implant length
C. A and B
D. None of the above
How to verify your CPD
Go online to https://https://https://https://sdmag.wpengine.com and click
on the CPD tab to access all our CPD
Q&As and certificates








Comments are closed here.