The dental psychological interface
This first article in a two-part series seeks to explore the influence psychological theory has had on the practice of dentistry by looking at the dentist/patient relationship and dental anxiety
There are four main domains where the workings of the mind have had an influence on our daily practice. These are: the dentist-patient relationship, dental anxiety, chronic oral facial pain and the stress of dental practice. In this article, I will address the first two domains and suggest ideas as to how both patients and the dental team would be better served by a more holistic body mind paradigm. In the next issue, I will discuss the final two influences. The duality of mind and body, first advocated in the 17th century by René Descartes, is finally beginning to find a home in Western medicine.
The influence of the mind on the development and progress of disease, both physical and psychological, is receiving the research attention that it merits. Descartes postulated that there was a real distinction between the immaterial mind and the material body. Although mind and body are ontologically distinct substances, they causally interact.
Psychology is defined in the Oxford dictionary as the scientific study of the human mind and its functions, especially those affecting behaviour. The etymology of the word is from modern Latin meaning the study of the soul. The history of psychology dates back to the Ancient Greeks who regarded it as a philosophy rather than a science. It was not until the late 1800s that it developed into a scientific subject.
Empathy and unconditional positive regard in the dental surgery invites us to treat others as we would like to be treated ourselves
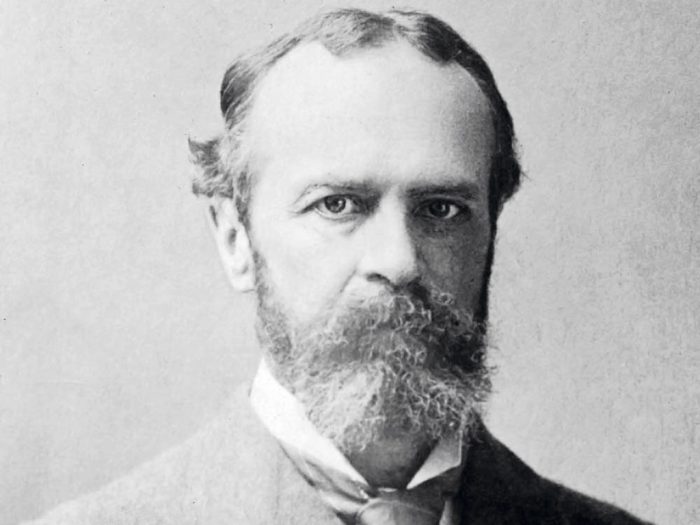
The first psychology lab was at the University of Leipzig where Wilhelm Wundt studied reaction times. The father of American psychology was William James who wrote The Principles of Psychology and was interested in conscious human experience. The dichotomy of thought in psychology made its appearance in Austria around the same period, with the work of Sigmund Freud on the unconscious. His psychoanalytic theory arose from work with hysterical patients were he proposed the unquiet mind derived from unresolved childhood conflicts.
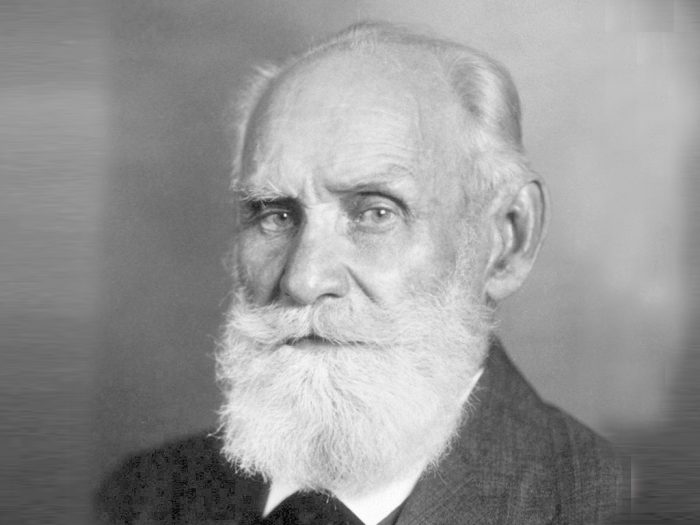
The work of the Russian psychologist Ivan Pavlov heralded in the age of behaviourism, his most famous experiment being Pavlov’s dogs showing classical conditioning. This was soon followed by Skinner and operant conditioning looking at behaviour in terms of actions and consequences. Carl Rogers’ theory gave birth to the third force in psychology known as humanistic psychology. It emerged as a paradigm to counteract the limitations of behaviourism and psychoanalysis.
Psychologists such as Rogers and Maslow were interested in the meaning and purpose of human behaviours. They were fascinated as to what conditions fostered the growth of the human person to self-actualise within the constraints of their own environment. The term cognitive psychology was first used by Ulric Neisser in 1967 and is a branch of psychology which is goal orientated and problem focused. The three main therapies arising from this way of thinking are:
- Albert Ellis’s rational emotive behaviour therapy (REBT)
- Aaron Beck’s cognitive therapy (CT)
- Donald Meichenbaum’s cognitive behaviour therapy (CBT)
The main principles under lying these therapies were first voiced by William James at the beginning of the 20th century: “Thoughts become perception, perception becomes reality. Alter your thoughts, alter your reality.”
Today, psychology is very much rooted in neuroscience and neurobiology. The advent of magnetic resonance imaging has provided a non-invasive way of examining the human brain. The amygdala, hippocampus, and medial prefrontal cortex have been shown to be involved in the stress response and in PTSD. Research in this domain is bringing understanding as to how therapies like eye movement desensitisation and reprocessing (EMDR) and brainspotting might work.
This brief introduction serves to demonstrate the plethora of knowledge that seeks to understand the human mind and human behaviour. The richness of psychological knowledge permeates into every area of society yet the primacy of this way of thinking is sometimes overlooked in the reductionist materialistic way that we teach our medical and
dental students.
Dentist-patient relationship
The work of Mills et al (2015) attempts to classify the main indicators of a good patient experience. In the UK, the NHS Patient Experience Framework highlights the Picker Principles of Patient-Centred Care as the optimum way to provide care. This form of care embraces much more than the daughter test as it invites us to see the other through the lens of compassion.
Patient-centred patient care has evolved from the philosophy of the humanistic psychologist Carl Rogers. Rogers believed that the patient is the expert in their own lives and, if given the opportunity, will self-actualise within their own environment. He used the metaphor of a potato in a darkened room sending out shoots towards a crack of light. If a patient is treated with empathy, unconditional positive regard and congruence within the dental domain then the framework for a positive patient experience is put in place.
This is fine rhetoric but words have no value unless they can be put into action. The following narrative, although not based in the dental surgery, involved a patient who sadly was in the end stages of oral cancer. His name has been altered to protect his identity. Many years ago, I had recourse to visit this man – let’s call him Bob – in hospital, he was dying from the ravaging effects of oral cancer. He was being fed through a peg tube and his breathing eased by a tracheostomy. This gentleman had been a rough sleeper for most of his life and had enjoyed solace from a homeless centre where I worked. On visiting him in his hospital room I brought him shower gel and soap to which he promptly replied: “What the hell are you bringing me these for? I need Guinness and fags!”
On exiting the room I put this request to the nursing sister; she looked at the patient and then myself and said to bring him some Guinness and some fags. On my next visit, I watched Bob syringe the Guinness into his peg tube and smoke his cigarette through his tracheostomy.
That nurse had treated Bob as a human being, she had given him dignity and respect. This man had lived on the streets where alcohol and cigarettes, for whatever reason, had been his only consolation. At this end stage of his life the nurse had looked on him with empathy and unconditional positive regard and bestowed upon him the dignity of being permitted to die with the tools that had enabled him to live. She, within the limits of her environment, had not allowed rigid protocols to undermine the humanity of the other.
Empathy and unconditional positive regard in the dental surgery invites us to treat others as we would like to be treated ourselves. It does not judge or stereotype our patients but treats each individual as unique. In this uniqueness, the encounters with our patients hold the potential of enriching both our lives and the life of the other. In my experience, kindness is the medium through which empathy is conveyed to the patient. Unconditional positive regard is the prising of the other for no other reason than they are our fellow travellers on this earthly sojourn. To hold the other in a positive light is to convey to them that they matter, they are not simply another extraction or a bridge to be fitted. They too have a place in society and their wellbeing is of prime importance to us.
The research of Sherman at the University of Washington Dental school shows that there is a decrease in clinical empathy over the four-year training course. This mirrors the work done by Chen (2012) on medical undergraduates. Research demonstrates that students who have a high level of empathy are more competent at history taking, have a higher physician and patient satisfaction, decreased malpractice litigation and are significantly better at motivating patients.
The importance of empathy in health care was emphasised in the Francis Report after the systemic failings at the Mid Staffordshire Foundation Trust. The GDC in their Preparing for Practice document highlight the importance of communication and professionalism in the training of undergraduates. Much research is needed in defining clinical empathy and discovering how best it may be taught.
Dental anxiety
The 2009 Adult Dental Health Survey, commissioned by the NHS Information Centre, revealed that 36 per cent of adults had moderate dental anxiety and 12 per cent were classified as being dentally phobic managing their anxiety by avoidance of all things dental. The impact of dental anxiety can have far-reaching consequences on a patients health and wellbeing, both psychologically and physically. Yet the literature reveals that there are no specific guidelines on the diagnosis or treatment of dental anxiety.
The work of Professor Tim Newton of King’s College London Dental Institute, Health Psychology Service and Art De Jongh of the Netherlands go along way to address this. Both authors offer a framework in which to classify dental anxiety and suggest different treatment modalities dependent of the level of anxiety. They propose that mild dental anxiety can and should be treated in the dental surgery by the dental team.
Research reveals that good interpersonal skills and empathy can of themselves decrease dental fear. Good communication enables the establishment of trust and a framework in which to carry out treatment. Precise information regarding the exact nature of treatment is essential to allay fears as is the establishing of a sense of control by adopting a stop signal. The “tell, show, do” technique has been about for more than 50 years and can be used for the simplest to the most complex treatment. There is also a place for the consideration of premedication and the use of nitrous oxide. The use of coping strategies such as distraction through visual or auditory stimuli and relaxation techniques all have part to play in mild dental anxiety management.
Hypnosis was first used in 1841 by the English physician James Braid and has been used in dentistry for well over half a century. It is a non-pharmacological method of inducing a trance-like state. In this state of altered consciousness, the patient is able to focus all of their attention on an image, thought or feeling and in so doing take their attention away from their feelings of anxiety. This method can also be very helpful in treating an overactive gag reflex, which is often found in dentally anxious patients. In order to aid the dental team in their treatment of patients with mild to moderate anxiety the website dentalfearcentral.org is an excellent resource for both staff and patients.
Patients who present with a moderate to severe level of dental anxiety should, in many cases, be referred to a secondary centre for the treatment of their dental anxiety. This secondary centre could be managed by a psychologist or a dentist with psychotherapy training (generic training or CBT training). The reason for this referral would be to assess the level of dental anxiety and also determine if there are any co-morbid psychological conditions.
In research done at Kings by Kani et al (2012), 37 per cent of the patients who had dental phobia were also shown to have high levels of generalised anxiety, 12 per cent had clinically significant depression and 12 per cent were shown to have suicide ideation. A referral centre that would enable assessment of dentally anxious patients would compliment a sedation service and offer patients definitive tailored treatment to address their dental anxiety.
A study done by Woolley in 2009 showed that individuals who are referred for sedation are highly anxious and fear a range of different dental stimuli. Yet previous research demonstrated that referring dentists to a sedation clinic did not consider psychological management for their patients. Sedation has, and always will have, a part to play in the management of dental anxiety but the only way to address the underlying issues is to complement the service with psychological interventions.
The study conducted by Kani et al (2012) showed that, of the 130 dentally phobic patients referred to the King’s College London Dental Institute, 79 per cent went on to have dental treatment without sedation. These patients were treated by CBT. This therapy has proven efficacy for the management of anxiety and depression. CBT is a synthesis of behaviour therapy and cognitive therapy which uses behaviour modification techniques and cognitive restructuring. It is a short-term therapy involving five to 10 sessions, usually of one hour duration. It is a collaborative enterprise and usually involves the patient doing homework.
Unlike many other psychotherapy treatments, it is a here and now therapy as what started a problem in the past is not often what keeps it going at the present time. The behaviour modification techniques involve such things as breathing exercises and in certain cases systematic desensitisation. The cognitive therapy involves identifying and challenging negative thoughts through the use of socratic questioning and the testing of hypothesis. The success of CBT is such that, in 2009, the Department of Health (England) recommended this therapy in conjunction with sedation services as a model of excellence in the management of dental fear.
The comprehensive assessment of patients allows different psychological interventions to be considered in the treatment of patients. The work of Art De Jongh has shown that were patients have a specific memory of dental trauma, EMDR may offer complete resolution of their dental phobia. EMDR stands for eye movement desensitisation and reprocessing and has been used extensively in people suffering from post traumatic stress disorder. The traumatic nature of memory formation in these individuals means that the memory of the trauma is unprocessed and the person is plagued by intrusive thoughts and flashbacks. By a process of bilateral stimulation either visual or auditory, the memory is accessed and desensitised of its affective content and negative cognitions. The memory is then accessed again and reprocessed with much less affect and a positive cognition. I have found this to be very successful in two or three visits where a phobia follows on from a specific dental trauma even when that trauma occurred many years previously.
Dental hypnosis has been revisited in the treatment of patients with moderate to severe dental anxiety. A study by Halsband et al (2015) has demonstrated that even brief dental hypnosis sessions can have an influence on the fear processing structures of the brain. Twelve dental phobic patients and 12 healthy control patients were tested by a 3T MRI whole body scanner observing brain activity changes after brief hypnosis. In the dental phobic group, dental fear was represented in the brain by increased activity in the left amygdala and bilaterally in the anterior cingulate cortex (ACC), insula and hippocampus (R<L).
- Mary Downie
- Tim Newton
- William James (Portrait 1890)
- Ivan Pavlov
- René Descartes
Amazingly, during hypnosis the scan revealed significantly reduced activity in these areas. In the healthy group of patients, no amygdala activity was observed. This study demonstrates objectively what hypnotherapists have been subjectively experiencing with their dentally phobic patients. In these times of great uncertainty, the wisdom of past ages is reemerging to show us a way forward without our heavy reliance on drugs.
The currency on which most psychological treatments thrive is time, unfortunately this is in short supply in busy NHS practices. In order to give dentally anxious patients the treatment that offers possible resolution of their condition, this paper proposes that psychological services must work in collaboration with dentistry.
This article has attempted to demonstrate that psychology can and does have an influence on the way we treat and manage our patients. The next article seeks to show how the treatment of chronic oral facial pain and the stress encountered in dental practice can be positively influenced by looking outward from the biomedical model. The wisdom of great scholars has been revisited as we seek to offer both our patients and the dental team a more balanced and productive way of practising.
References
Adult Dental Health Survey 2009, NHS Digital.
Chen DC, Kirshenbaum DS, Yan J, Kirshenbaum E, Aseltine RH. Characterizing changes in student empathy throughout medical school.
Med Teach. 2012;34(4):305-11. doi: 10.3109/0142159X.2012.644600.
DeJongh A, Adair P, Meijerink-Anderson M. Clinical Management of Dental Anxiety: What works for whom? International Dental Journal (2005) 55, 73-80
De Jongh. A, Van Den Oord. H, Ten Broeke, E. Efficacy of Eye Movement Desensitization and Reprocessing in the Treatment of Specific Phobias: Four Single-Case Studies on Dental Phobia Journal of Clinical Psychology, Vol. 58(12), 1489–1503 (2002)
GDC Publications Preparing for Practice.
Halsband, Ulrike; Wolf, Thomas Gerhard; NLM Functional changes in brain activity after hypnosis in patients with dental phobia Journal of physiology, Paris109.4-6 (Dec 2015): 131-142.
Kani E, Asimakopoulou K, Daly B, Hare B, Lewis J, Scambler S, Scott S, and Newton JT. Characteristics of patients attending for cognitive behavioural therapy at one UK specialist unit for dental phobia and outcomes of treatment. British Dental Journal Volume 219 No. 10 Nov 27 2015
Mills I, Frost J, Kay E, and Moles DR. Person-centred care in dentistry – the patients’ perspective. British Dental Journal 218, 407 – 413 (2015) Published online: 10 April 2015 | doi:10.1038/sj.bdj.2015.248
Newton T, Asimakopoulou K, Daly B, Scambler S, and Scott S. The management of dental anxiety: time for a sense of proportion? British Dental Journal 2012; 213: 271-2 74
Sherman J and Cramer A. Measurement of Changes in Empathy During Dental School. Journal of Dental Education Vol 69 Number 3
Woolley SM, Summary of: Who is referred for sedation for dentistry and why? Published online: 28 March 2009 | doi:10.1038/sj.bdj.2009.233
About the author
Mary graduated from Glasgow University in 1980 and from the Open University in 2001. She obtained a postgraduate diploma in counselling and psychotherapy from Stirling University in 2013. She has enjoyed a plethora of experiences in dentistry both in the UK and abroad.She especially enjoyed her post in Glasgow University teaching oral surgery. Mary is now in full-time psychotherapy practice but would like to combine psychotherapy and dentistry if the right post became available.
CPD responses closed
The CPD quiz for this article is now closed. Please check the listings for the current quizzeslistings




Comments are closed here.