Pain management
In the May/June issue, Dr Aditi Desai explained how to introduce dental sleep medicine (DSM) into your practice. Now, she and Dr Mayoor Patel explain the link between sleep-disordered breathing and pain
In recent years dentistry has advanced from more than just oral health to overall health. One of the outcomes of this is dental sleep medicine – the management of snoring and obstructive sleep apnoea (OSA), both of which are classed as a sleep-related breathing disorder (SRBD). Approximately one in 30 people in the UK complain about headaches each year and it is estimated that around 1.5 million adults have OSA, although only around 330,000 are currently diagnosed and treated. These numbers are increasing as obesity levels rise in adults and children. In a UK cross-sectional study, 12 per cent of children were found to be habitual snorers and 0.7 per cent were found to have obstructive sleep apnoea 1.
Understanding sleep apnoea and snoring
OSA is a sleep-related respiratory condition, leading to intermittent cessations of breathing due to a narrowing or closure of the upper airway during sleep. Symptoms of OSA often include excessive daytime sleepiness, snoring, and witnessed apnoeas or hypopnoeas (collapse of the airway leading to breathing cessations). Although OSA is thought to be a disorder affecting the overweight or obese, it can affect anyone and is estimated to affect 1.5 million adults in the UK, men, women and children.
Craniofacial pain and TMD
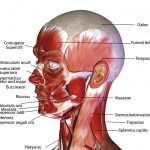
Temporomandibular joint dysfunction (TMD) refers to a group of disorders affecting the temporomandibular joint (TMJ), masticatory muscles and the associated structures (Fig 1). Common symptoms of TMD include pain, limited mouth opening and joint noises (also known as clicking of the jaw).
TMD symptoms affect up to 25 per cent of the population with only 5 per cent seeking medical help for their symptoms – they simply put up with the pain or can’t find a treatment 2. TMD can occur at any age but is more common among women and those between the ages of 20 and 50.
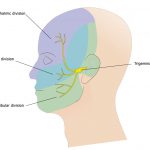
The main sensory nerve system running through the head is the trigeminal nerve system (Fig 2) and accounts for 90 per cent of all the sensory input into the entire nervous system. Because of this we can explain why TMD can sometimes lead to debilitating symptoms for those who suffer from this condition. Many patients will seek treatment for craniofacial pain due to recurring migraines, but 90 per cent of headaches are really caused by disorders in the facial muscles and nerves.
- Figure 1 – Muscles of the face including the masticatory muscles
- Figure 2 – Trigeminal nerve – the three different innervation areas of the head
- Figure 3 – Continuous positive airway pressure (CPAP) machine in use
A connection between sleep apnoea and pain
As research continues to advance we see a clear connection between sleep-disordered breathing, craniofacial pain and TMD, which requires proper evaluation and diagnosis by dental and medical teams. Essentially, it is the dental clinician who will often evaluate, refer and possibly manage these issues which impact such a large percentage of the population.
There is ample evidence to suggest that sleep apnoea and pain are related, but many questions still remain. One main trend emerging pertains to the directionality and mechanisms of the association of sleep apnoea and chronic pain. It appears that sleep disturbance may impair key processes that contribute to the development and maintenance of chronic pain, including joint pain (TMD). In a recent study, sleep disturbance and pain were connected. It determined that pain not only has direct effects on the person’s health, but also an association with sleep disturbances
Many studies have suggested that experimental sleep disruption results in enhanced pain perception and interactions between sleep and pain. It is suggested that experimental sleep disruption results in enhanced pain perception, that poor sleep is correlated with elevated pain severity in chronic pain patients and that in the general population, individual differences in sleep impact on subsequent pain. A study published in the European Journal of Pain stated that sleep fragmentation among healthy adults resulted in subsequent decrements in endogenous pain inhibition 3.
With an evident relationship, we look to understand that clenching or grinding of one’s teeth is a way for the brain to protect itself from suffocation during sleep 4,5,6,7,8. The screening process is important in helping us identify bruxism as either a cause of TMJ/craniofacial pain or a protective mechanism in sleep disordered breathing 9,10,11,12. By identifying this link between the three conditions we can properly manage each disorder.
Dental solutions for proper treatment
Patients who suffer from severe sleep apnoea might opt for surgery for treatment. However, sleep apnoea surgeries have a history of causing the patient excruciating pain. The gold standard for severe OSA patients is use of the continuous positive airway pressure (CPAP) machine (Fig 3), with success ranging in various studies from 90 to 95 per cent. However, the problem with CPAP treatment is patient non-compliance and intolerance. When people return home, there is a good chance they just won’t use their machine 13.
There are challenges posed by sleep apnoea and craniofacial pain which span the research spectrum – from causes to diagnosis through treatment and prevention. It is important for us all to work together to gain a better understanding of sleep apnoea, the TMJ and muscle disease process and craniofacial pain, as well as improving quality of life for people affected by these disorders.
Dentists see their patients more often than family doctors, as it is recommended that patients visit a dentist at least twice a year. Since we are typically seeing our patients more often, it is important to understand sleep apnoea, TMD and craniofacial pain, as well as gaining an understanding of the right questions to ask.
As only one out of 20 UK patients suffering from pain actually seek treatment and that 85 per cent of patients with sleep apnoea either don’t or do not know where to seek help, it is vital that we ask the right questions in order to gain a proper diagnosis. If they are suffering from pain they might not realise the solution can be found at the dental practice:
- Palliative care – medications to better improve a patient’s pain
- Changing a patient’s diet – this would include soft foods or foods that don’t overextend the jaw or cause pressure on the head. For sleep apnoea it would include foods to help in weight control or loss
- Oral appliance therapy and orthodontics – offer a way to realign the jaw and teeth to relieve pressure on the face and jaw while preventing the tongue from falling over the airway.
Dentists hold the key to successful management of sleep apnoea and pain among patients who might think a solution is not possible. It is our responsibility to continue to advance our knowledge of various areas of dentistry we might not be exposed to in our undergraduate training – there is more out there than we were taught.
Advanced education
As dentists we must look to better understand sleep apnoea, snoring and craniofacial pain in order to provide our patients with the care they need to live a good quality of healthy and happy lives. Further education through lectures and seminars becomes essential with a wide range of continuing education courses available. Only through education can we continue to offer the help that patients with this debilitating condition need.
Since this is not a subject that is covered in the undergraduate curriculum, postgraduation certification in dental sleep medicine and craniofacial pain allows the whole team to engage with various medical and dental specialities to offer the optimum management options to these patients.
The British Society of Dental Sleep Medicine (BSDSM) has for many years run one-day dental sleep medicine courses which have proved very popular. As well as providing an overview of sleep disordered breathing, advising how to identify and safely assess patients at risk and explaining treatment and management options, the courses now include a module on temporomandibular joint dysfunction and craniofacial pain.
The BSDSM also provides a wealth of information on snoring and OSA, advice on treatment options for the public, patients and healthcare professionals and promotes discussion on dental sleep medicine. For more information, visit www.bsdsm.org.uk
About the author
Dr Mayoor Patel DDS, MS, D.ABDSM, DABOP, DABCP, DABCDSM, DAPPM, RPSGT, FAAOP, FICCMO, FAACP, FAGD is owner of the Craniofacial Pain Center of Georgia in the US, co-owner of MAP Laboratory LLC and Director of Clinical Education at Nierman Practice Management. He is a board member of the American Board of Craniofacial Pain, the American the Academy of Craniofacial Pain, the American Board of Craniofacial Dental Sleep Medicine and a director of the Georgia Association of Sleep Professionals.
Dr Aditi Desai BDS, MSc is president of the British Society of Dental Sleep Medicine (BSDSM). She has accreditation from the European Academy of Dental Sleep Medicine and serves on the Council of the Odontological and Sleep Section at the Royal Society of Medicine (RSM). Dr Desai limits her practice predominantly to the management of sleep disorders. Based in Harley Street and London Bridge Hospital, she works with other eminent physicians and ENT consultants as part of a multidisciplinary team of like-minded professionals with special interest in sleep medicine. She is an invited speaker at the RSM, the Royal College of Surgeons of England, the British Sleep Society, the British Dental Association and many other organisations. She has published several articles in dental journals on dental sleep medicine and lectures on the subject in the UK and internationally.
References
1. Ali NJ, Pitson DJ, Stradling JR. Snoring, sleep disturbance, and behaviour in 4-5 year olds. Arch Dis Child 1993; 68(3): 360-6.
2. Murphy, M.K., et al., Temporomandibular Joint Disorders: A Review of Etiology, Clinical Management, and Tissue Engineering Strategies. The International Journal of Oral & Maxillofacial Implants, 2013. 28(6): p. e393.
3. Edwards, R., et al., Sleep continuity and architecture: Associations with pain-inhibitory processes in patients with temporomandibular joint disorder. European Journal of Pain, 2009. 13(10): p. 1043-1047.
4. Ng, D.K., et al., Prevalence of sleep problems in Hong Kong primary school children: A community-based telephone survey. Chest, 2005. 128(3): p. 1315-1323.
5. Phillips, B., et al., Effect of sleep position on sleep apnea and parafunctional activity. Chest, 1986. 90(3): p. 424-429.
6. Bailey, D.R., Sleep disorders. Overview and relationship to orofacial pain. Dental clinics of North America, 1997. 41(2): p. 189-209.
7. Hosoya, H., et al., Relationship between sleep bruxism and sleep respiratory events in patients with obstructive sleep apnea syndrome. Sleep Breath, 2014. 18(4): p. 837-44.
8. Saito, M., et al., Temporal association between sleep apnea-hypopnea and sleep bruxism events. J Sleep Res, 2013.
9. Blanco Aguilera, A., et al., Relationship between self-reported sleep bruxism and pain in patients with temporomandibular disorders. J Oral Rehabil, 2014. 41(8): p. 564-72.
10. Manfredini, D. and F. Lobbezoo, Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 2010. 109(6): p. e26-e50.
11. Unell, L., et al., Changes in reported orofacial symptoms over a 10-year period as reflected in two cohorts of 50-year-old subjects. Acta Odontol Scand, 2006. 64(4): p. 202-8.
12. Ahlberg, K., et al., Perceived orofacial pain and its associations with reported bruxism and insomnia symptoms in media personnel with or without irregular shift work. Acta Odontol Scand, 2005. 63(4): p. 213-7.
13. Richard, W., et al., Acceptance and long-term compliance of nCPAP in obstructive sleep apnea. European Archives of Oto-Rhino-Laryngology, 2007. 264(9): p. 1081-1086.
Verifiable CPD Questions
Aims and Objectives
To explain the prevalence of obstructive sleep apnoea (OSA) in the UK population and the numbers diagnosed and treated
- To provide a concise explanation of snoring and OSA
- To explain the causes of craniofacial pain and temporomandibular joint dysfunction (TMD) and its symptoms
- To make the link between sleep apnoea and pain
- To explain how dentists can help the management of OSA and pain in their patients
- To identify the need for post-graduate training in dental sleep medicine.
Learning outcomes
- A basic understanding of sleep apnoea, craniofacial pain and temporomandibular joint dysfunction
- Sufficient knowledge of how dental sleep medicine can help patients manage OSA and pain to decide whether to undertake formal training
- Know where to access training in dental sleep medicine and learn more about the management of craniofacial pain and TMD.


Comments are closed here.