Comfortably numb
Dr Laura Fee explores the controversies surrounding local anaesthetics and the medically complex patient
Local anaesthetics interrupt neural conduction by inhibiting the influx of sodium ions through channels within neuronal membranes. When the neuron is stimulated, the channel is activated and sodium ions can diffuse into the cell, triggering depolarisation. Following this sudden change in membrane voltage, the sodium channel assumes an inactivated state and further influx is denied while active transport mechanisms return sodium ions to the exterior.
After this repolarisation, the channel assumes its normal resting state. Local anaesthetics have the greatest affinity for receptors in the sodium channels during their activated and inactivated states rather than when they are in their resting states 1, 2.
Pharmacology
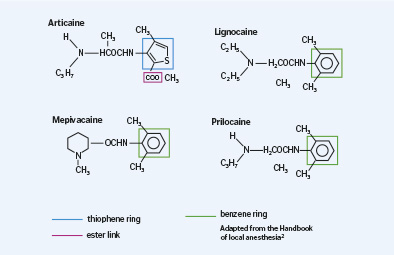
Local anaesthetics consist of three components that contribute necessary clinical properties:
- Lipophilic aromatic ring – improves lipid solubility of the compound
- Intermediate ester/amide linkage
- Tertiary amine.
Articaine consists of an amide group and an ester link. It has a thiophene ring instead of a benzene ring, as seen in the chemical structure of lignocaine. The thiophene ring improves its lipid solubility. Therefore in some studies articaine shows better potential for penetrating through the neuronal sheath and membrane when compared with other local anaesthetics 3.
The dissociation constant of an anaesthetic affects its onset of action. The lower the pKa values, the greater the proportion of uncharged base molecules can diffuse through the nerve sheath. Articaine has a pKa of 7.8, whereas lignocaine has a pKa of 7.9. This proves important when a local anaesthetic is administered to anaesthetise inflamed tissues, where the ph of the tissues is reduced 4. Articaine has a half-life of 20 minutes, whereas lignocaine has a half-life of 90 minutes. Therefore, articaine presents less risk for systemic toxicity during lengthy dental treatments when additional doses of anaesthetic are administered 5.
Comparison between articaine and lignocaine
Some studies argue that there is no significant difference in pain relief provided by 2 per cent lignocaine and 4 per cent articaine where both formulations contain adrenaline 6. However, a recent systematic review demonstrated a different conclusion 7. This review showed that when considering successful infiltration anaesthesia, 4 per cent articaine solution containing adrenaline was almost four times greater than a similar volume of 2 per cent lignocaine also containing adrenaline. Other studies have stated that 4 per cent articaine offers superior levels of anaesthesia in the anterior maxillary region when compared to 2 per cent lignocaine, however this level of superiority appears less significant in the maxillary molar region 8.
There is evidence to support that articaine is more effective in the maxillary posterior region when compared with lignocaine when tissues are inflamed 9. However, there is insufficient evidence to suggest a similar level of superiority for mandibular teeth, where the solution has been administered with the inferior alveolar nerve block technique 10.
The additive administration of lignocaine using the IANB technique and buccal infiltration with articaine could potentially increase the level of pulpal anaesthesia achieved in the mandibular molar and premolar area 11. The inclusion of adrenaline in 4 per cent articaine is considered critical in achieving its profound anaesthesia 12.
Brandt et al demonstrated that articaine was superior when administered using the inferior alveolar nerve block technique (IANB) 7. However, it must be stressed that the potency of the agent administered via the inferior alveolar block was considerably lower than the potency administered by the infiltration technique. It was shown that neither articaine or lignocaine demonstrated superiority over the other when administered to symptomatic teeth. It is important to recognise the limitations in this study of comparing a 4 per cent solution of articaine with a 2 per cent solution of lignocaine 7. Other studies also reported no difference between articaine and lignocaine when using the IANB technique while treating symptomatic teeth 11,13.
Interestingly, it has been demonstrated that 4 per cent articaine with 1:100,000 adrenaline administered using the buccal infiltration technique had a significantly faster onset of pulpal anaesthesia when compared with the inferior alveolar nerve block. Therefore, dentists can consider the use of articaine administered by a buccal infiltration as an alternative to the inferior alveolar nerve block when anaesthetising the mandibular first molar 14. Another study also concluded that articaine delivered by buccal infiltration alone was more effective than lignocaine administered by the inferior alveolar technique when anaesthetising mandibular first molar teeth 15.
Paraesthesia
In 2010, Garisto et al reported 248 cases of paraesthesia after dental treatment 16. Most cases involved mandibular nerve blocks and, in 89 per cent of cases, the lingual nerve was damaged. Paraesthesia was shown to be 7.3 times more likely with 4 per cent articaine when compared with lignocaine. Similar findings were reported by Hillerup et al, who demonstrated greater neural toxicity of 4 per cent compared to 2 per cent articaine. Therefore, it might be advisable to limit the use of 4 per cent articaine to infiltrations and avoid for nerve blocks 17.
Articaine has also been shown to be superior for infiltrations in the mandible and does not cause neural toxicity unless injected near the mental nerve 18.
Paraesthesia has been associated with the use of local anaesthetics, especially when administered using the inferior alveolar nerve block technique 19. Observational research performed in Denmark reported a 20-fold greater risk of nerve injury when articaine was used compared with other local anaesthetics and administered via the IANB technique 17. Given that articaine is less neurotoxic than other anaesthetics, the findings of this research were unexpected 20. It is important to consider that the aetiology of paraesthesia may be the result of a needle injury to the lingual and inferior alveolar nerve. Factors including intra-neural haematoma, extra-neural haematoma, oedema and chemical neurotoxicity of articaine may also play a role 21.
Dentists must also consider the ‘Weber effect’ 22. This occurs when a new product is launched onto the market and is scrutinised more closely. Immediately after 4 per cent articaine containing 1:100,000 adrenaline was introduced, there was a significantly increased incidence of paraesthesia. But, two years later, a reduction was recorded despite an increased number of cartridges being sold 21.
The literature reports that the lingual nerve is more frequently damaged than the inferior-alveolar nerve. Approximately 70 per cent of permanent nerve damage is sustained by the lingual nerve, whereas a 30 per cent occurrence was recorded affecting the inferior alveolar nerve 23. Current data indicates that 85-94 per cent of non-surgical paraesthesia caused by local anaesthetics recovers within two months. After a two month period, two thirds of those patients whose paraesthesia has not resolved will never completely recover 23.
Articaine is also used in areas of medicine such as plastic and reconstructive surgery, ophthalmology and orthopaedic surgery. It is interesting that there are no reports of paraesthesia from articaine following its use in medicine. Is it possible that articaine only affects nerves supplying the oral cavity and specifically the lingual nerve? It is thought that paraesthesia affects the lingual nerve twice as much as the inferior alveolar nerve due to the fascicular pattern of the injection site. Also, when a patient opens their mouth for treatment the lingual nerve is stretched and more anteriorly placed; this decreases its level of flexibility, which is needed to deflect the needle. During administration, the barbed needle can damage the inferior alveolar or lingual nerve during withdrawal 24.
Interestingly, in 2006 – when Hillerup raised concerns that articaine was responsible for neurosensory disturbances – it was found that 80 per cent of all these reports came from Denmark. It is worth noting that, at the time, the Danish population was approximately 5.6 million compared with 501 million in the wider EU community. This research led to the Pharmacovigilance Working Party of the European Union conducting an investigation involving 57 countries and more than 100 million patients treated with articaine. The conclusion was emphatic, stating that all local anaesthetics may cause nerve injury. They estimated that the incidence of sensory impairment following administration of articaine was one in every 4.6 million treated patients. Therefore, no medical evidence existed to prohibit the use of articaine and the safety profile of the drug remained unchanged.
It is worth considering that, before articaine was introduced to the USA, the incidence of permanent nerve damage from inferior alveolar nerve blocks was 1:26,762. In 2007, Pogrel also concluded that nerve blocks can cause permanent damage regardless of which anaesthetic agent is used. Both articaine and lignocaine have been associated with this phenomenon in proportion to their use.
Negative side-effects
Articaine can result in restlessness, anxiety, light-headedness, convulsions, dizziness, tremors, drowsiness and depression 13. Ocular complications have been reported due to interference with sensory and motor pathways 25. Other adverse effects include headaches, facial oedema and gingivitis 13. Skin rashes with itching after administration of articaine have also been cited in the literature 26. Skin necrosis on the chin has also been reported after administration of 4 per cent articaine using the IANB technique 27.
With regards to the cardiovascular system, 4 per cent articaine can decrease cardiac conduction and excitability. Complications such as reduced myocardial contractility, peripheral vasodilation, ventricular arrhythmia, cardiac arrest and, rarely, death have been reported in the literature 28. It is important to exercise caution in patients with severe hepatic impairment. However, the rapid breakdown of articaine into inactive metabolites results in low systemic toxicity 29.
Conclusions on articaine
Since 1973, there have been more than 200 papers published on articaine. Virtually all of these studies have concluded that articaine is as effective and safe as other comparable local anaesthetic agents such as lignocaine, mepivacine or prilocaine. It was shown that articaine is the least likely anaesthetic to induce an overdose caused by administration of too many cartridges. No significant difference in pain relief has been observed between adrenaline containing formulations of 4 per cent articaine and 2 per cent lignocaine.
The time of onset and duration of anaesthesia for 4 per cent articaine is comparable to other commercially available local anaesthetics. Furthermore, the majority of studies have indicated that the incidence of complications including paraesthesia are equal for lignocaine and articaine. The FDA has approved articaine 4 per cent with adrenaline 1:100,000 to age four years in paediatric patients.
The popularity of articaine cannot be disputed within the dental profession. In the USA in 2009, 41 per cent of all dental local anaesthetic used was articaine. In 2012, the market share for articaine in Germany was 97 per cent and in the same year, it was shown that 70 per cent of dentists use articaine in Australia.
Adrenaline-containing anaesthetics
Adrenaline causes constriction of blood vessels by activating alpha-1 adrenergic receptors. It aids hemostasis in the operative field and delays absorption of the anaesthetic. This delayed absorption decreases the risk of systemic toxicity and lengthens its duration of action. Adrenaline can cause considerable cardiac stimulation due to its affect as a beta-1 adrenergic agonist 30.
Cardiovascular influences
Adrenaline is an agonist on alpha, beta-1 and beta-2 receptors. It is a vasoconstrictor as the tiny vessels in the submucosal tissues contain only alpha receptors 31. There is much debate regarding the influence of adrenaline on patients with cardiovascular disease. Dionne et al studied the influence of three cartridges of the American formulation Lidocaine with adrenaline 1:100,000. Submucosal injection of this dosage increased cardiac output, heart rate and stroke volume. Systemic arterial resistance was reduced and mean arterial pressure remained unchanged 32.
Likewise, Hersh et al observed similar results following the administration of articaine containing 1:100,000 and 1:200,000 adrenaline. Although the influence of adrenaline reported by Hersh et al was minor, it is noteworthy that all 14 participants were healthy and taking no medication, yet two of these patients experienced palpitations 33.
A dose of approximately two cartridges of lignocaine containing adrenaline 1:80,000, is the most conservative and frequently cited dose limitation for patients with significant cardiovascular disease. Ultimately, the decision requires the dentist to practise sound clinical judgement and to discuss any concerns with that patient’s doctor if necessary. Peak influences of adrenaline occur within five to 10 minutes following injection and they decline rapidly 33.
Another practical suggestion is to determine the dosage based on patient assessment. If the medical status of a patient is questionable, a sensible protocol is to record baseline heart rate and blood pressure preoperatively and again following administration of two cartridges of lignocaine containing 1:80,000 adrenaline. If the patient remains stable, additional doses may be administered, followed by a reassessment of vital signs 30.
Hypertension
After administering one to two cartridges of adrenaline-containing local anaesthetic with careful aspiration and slow injection and the patient exhibits no signs or symptoms of cardiac alteration, additional adrenaline containing local anaesthetic may be used. A safe option preferred by some dentists is to firstly use a minimal amount of adrenaline-containing local anaesthetic and then supplement as necessary with an adrenaline-free anaesthetic 34.
The risk of the anaesthesia wearing off too soon, resulting in the patient producing elevated levels of endogenous adrenaline because of pain, would be much more detrimental than the small amount of adrenaline in the dental anaesthetic 35.
Drug interactions
Beta-adrenergic blocking drugs increase the toxicity of adrenaline-containing local anaesthetics. It inhibits enzymes in the liver and decreases hepatic blood flow. Therefore, it is advisable not to give large doses of local anaesthetic to patients on beta blockers. There have been multiple reports of stroke and cardiac arrest within the literature 36. Slow administration and aspiration can also help prevent undesirable reactions 37.
Judicious use of adrenaline is recommended for patients medicated with nonselective beta blockers. Unlike selective agents that only block beta-1 receptors on the heart, nonselective agents also block vascular beta-2 receptors. In this case, the alpha agonist action of adrenaline becomes more pronounced and both diastolic and mean arterial pressures can become dangerously increased. This is often accompanied by a sudden decrease in heart rate. Significant consequences of this interaction are well documented 38.
The interaction with beta blockers follows a time course similar to that observed for normal cardiovascular responses to adrenaline. It commences after absorption from the injection site, peaks within five minutes and declines over the following 10-15 minutes. Adrenaline is not contraindicated in patients taking nonselective beta blockers, but doses must be kept minimal and monitoring of blood pressure advisable 39.
Verapamil, which is a popular calcium channel blocker, increases the toxicity of 2 per cent lignocaine. As for patients taking beta-adrenergic blocking drugs, two cartridges should be the limit 40. With regards to bupivacaine, calcium channel blockers enhance the cardiotoxicity of this longer acting anaesthetic 41.
Antihypertensives are the main cardiovascular drugs that interact with anaesthetics containing adrenaline. Theoretically, beta-blockers, diuretics and calcium-channel blockers may all result in adverse reactions when used with adrenaline-containing local anaesthetics 42.
Adrenaline causes alpha and beta-adrenergic agonism. Alpha-adrenoreceptor stimulation results in vasoconstriction of peripheral blood vessels, whereas beta-adrenoreceptor stimulation decreases vascular resistance due to vasodilation of vessels in the liver and muscles, therefore reducing diastolic blood pressure. If beta-effects are blocked, the alpha-adrenergic stimulation leads to an unopposed increase in systolic blood pressure triggering a cerebrovascular accident.
Therefore, if more than one to two cartridges are needed in such patients, adrenaline-free solutions should be administered. An advantage, however, of beta-adrenoreceptor blockers in dental patients is that the heart is protected from the elevation in rate produced by beta-adrenergic stimulation from exogenous adrenaline 43.
Diuretics can affect the metabolic actions of adrenaline. Increased levels of adrenaline reduces the plasma concentration of potassium 44. These reductions have been documented in patients receiving dental local anaesthetics containing adrenaline 45.
In patients undertaking oral surgery procedures who are taking non-potassium-sparing diuretics, there have been incidences of adrenaline-induced hypokalaemia 44. It should remembered that calcium channel blocking drugs may also increase adrenaline-induced hypokalaemia 46.
| AGENT | CONC W/V | CONC MG/ML | MAX DOSE MG/KG | DOSE ML/KG | MG MAX DOSE | CARTRIGES |
|---|---|---|---|---|---|---|
| BUPIVACAINE 0.5% | 0.5 | 5 | 1.3 | 0.26 | 90 | 8 |
| LIDOCAINE 2% | 2 | 20 | 4.4 | 0.22 | 300 | 6 |
| MEPIVACAINE 2% | 2 | 2 | 4.4 | 0.33 | 300 | 6 |
| ARTICAINE 4% | 4 | 40 | 7 | 0.18 | 500 | 5 |
| PRILOCAINE 3% | 3 | 30 | 5 | 4.4 | 400 | 6 |
| MEPIVACAINE 3% | 3 | 30 | 4.4 | 0.15 | 300 | 4 |
| PRILOCAINE 4% | 4 | 40 | 5 | 0.13 | 400 | 4 |
| AGENT | CONCENTRATION | TRADE NAME |
|---|---|---|
| BUPIVACAINE | 0.5% | MERCAINE |
| MEPIVACAINE | 2% | LIGNOSPAN |
| LIDOCAINE | 2% | SCANDONEST |
| PRILOCAINE | 3% | SEPTANEST |
| ARTICAINE | 4% | CITANEST |
| MEPIVACAINE | 3% | SCONDONEST |
| PRILOCAINE | 4% | CITANEST |
Angina pectoris and post-myocardial infarction
The use of adrenaline containing local anaesthetics is advisable as part of a stress reduction protocol. The dosage of the adrenaline should be limited to that contained in two cartridges of lignocaine 2 per cent 1:80,000 adrenaline. For patients with unstable angina, a recent myocardial infarction less than six months previously or a recent coronary artery bypass graft surgery within three months warrant all elective dental treatment to be deferred 47. If emergency treatment is imperative, stress-reduction protocols with anti-anxiety agents are advisable with a limitation of two cartridges of adrenaline containing anaesthetic 48.
As part of a stress reduction protocol, the Wand allows the dentist to administer local anaesthetic with a non-threatening handpiece. The anaesthetic syringe is often the principle cause of stress for patients as it is considered by many as the most uncomfortable part of dental treatment. The Wand helps deliver a computer-regulated flow of anaesthetic that enables pain-free dental anaesthesia for the different types of injections. This can help to make the patient less anxious.
Cardiac dysrhythmia
Elective dentistry should be postponed in patients with severe or refractory dysrhythmias until they are stabilised.
It is safe to limit the local anaesthetic dose to two cartridges of lignocaine 2 per cent containing 1:80,000 adrenaline 49. The use of periodontal ligament or intraosseous injections using an adrenaline-containing local anaesthetic is contraindicated 50.
Congestive heart failure
Patients taking digitalis glycosides, such as digoxin, should be carefully monitored if adrenaline-containing anaesthetics are administered as an interaction between these two drugs can trigger dysrhythmias. Patients taking long-acting nitrate medications or taking a vasodilator medication may show decreased effectiveness of the adrenaline and therefore may experience a shorter duration of dental local anaesthesia 48.
Cerebrovascular accident
Following a stroke, it is recommended that dental treatment be deferred due to the significantly elevated risk of recurrence. Following a six-month interval, dental procedures can be rescheduled with the use of adrenaline-containing local anaesthetics. If the stroke patient has associated cardiovascular problems, the dosage of local anaesthetic with vasoconstrictor should be kept to a minimum 48.
Asthma
Stress can precipitate an asthma attack, making stress-reduction protocols essential. Conservative use of local anaesthetics containing adrenaline is advised. The Food and Drug Administration warn that drugs containing sulfites can cause allergic reactions in susceptible individuals 51.
Some studies suggest that sodium metabisulfite, which is an antioxidant agent used in dental local anaesthetic, may induce asthma attacks 52. Data is limited on the incidence of this reaction and even in sulfite-sensitive patients, it appears to be an extremely small risk. Indications are that more than 96 per cent of asthmatics are not sensitive to sulfites and those who are sensitive are usually severe, steroid-dependent asthmatics 53.
Perusse and colleagues concluded that local anaesthetic with adrenaline can be safely used in patients with nonsteroid-dependent asthma. However, until we learn more about the sulfite sensitivity threshold, conservative use of local anaesthetic with adrenaline in corticosteroid-dependent asthma patients is advisable. This is due to their higher risk of sulfite allergy and the possibility that an unintentional intravascular injection might occur, causing a severe asthmatic reaction in a sensitive patient 54. However, in recent times, the results of these older studies have been regarded as questionable by many in the profession.
Hepatic disease
In patients with chronic active hepatitis or with carrier status of the hepatitis antigen, local anaesthetic doses must be kept to a minimum. In patients with more advanced cirrhotic disease, metabolism of local anaesthetics may be significantly slowed, resulting in increased plasma levels and complications from toxicity reactions. Local anaesthetic dosage may need to be decreased and the time lapse between injections extended 55.
Diabetes
Some patients experience dramatic swings between hyperglycemia and hypoglycemia and, therefore, the use of adrenaline-containing anaesthetics should be reduced due to the risk of adrenaline-enhanced hypoglycemia 48.
Cocaine
The major concern in patients abusing cocaine is the significant danger of myocardial ischemia, cardiac dysrhythmias and hypertension. Some researchers recommend deferral of dental treatment for 24 to 72 hours 56.
Tricyclic antidepressants
One to two cartridges of adrenaline-containing local anaesthetic can be safely administered to patients taking these drugs. However, careful observation at all times for signs
of hypertension is necessary due to enhanced sympathomimetic effects 57.
HIV
Protease-inhibitor drugs have been shown to increase the plasma levels of lignocaine potentially increasing cardiotoxicity 58.
Parkinson’s disease
Athough there is no data regarding the influence of the anti-Parkinson drug entacapone, caution is advised while using adrenaline-containing anaesthetics. Three cartridges of 2 per cent lignocaine with 1:80,000 adrenaline is the recommended upper limit in adults 59.
Local anaesthetic reversal
A local anaesthetic reversal agent has been introduced that effectively reverses the influence of adrenaline on submucosal vessels. Phentolamine (Ora Verse) is an alpha receptor blocker formulated in dental cartridges 60.
In the future, this may prove useful for some medically compromised patients such as diabetics or elderly patients for whom adequate nutrition may be hindered by prolonged numbness. However, currently this reversal agent is not available in the UK or Ireland.
About the author
Dr Laura Fee graduated with an honours degree in dentistry from Trinity College, Dublin. During her studies, she was awarded the Costello medal for undergraduate research on cross-infection control procedures. She is a member of the Faculty of Dentistry at the Royal College of Surgeons and, in 2013, she completed the Certificate in Implant Dentistry with the Northumberland Institute of Oral Medicine and has since been awarded the Diploma in Implant Dentistry with the Royal College of Surgeons, Edinburgh. Laura is currently completing the Certificate in Minor Oral Surgery with the Royal College of Surgeons, England. She has also been involved with undergraduate teaching in the School of Dentistry, Belfast where she has an honorary oral surgery contract.
References
-
Berde CB, Strichartz GR. Local anesthetics. In: Miller RD, Eriksson LI, Fleisher LA et al. Miller’s Anesthesia. 7th ed. Philadelphia, Pa: Elsevier, Chuchill Livingstone, 2009.
-
Katzung BG, White PF. Local anesthetics. In:Katzung BG, Masters SB, Trevor AJ, editors. Basic and Clinical Phamacology. 11th ed. New York, NY: Mc Graw-Hill Companies Inc; 2009
-
Malamed SF, Gagon S, Leblanc D. The efficacy of articaine: a new amide local anesthetic. J Am Dent Assoc 2000; 131:635-642
-
Kakroudu SHA, Mehta S, Millar BJ. Articaine Hydrochloride: Is it the solution? Dent Update 2015; 42:88-93
-
Becker DE, Reed KL. Essentials of local anesthetic pharmacology. Anesth Prog 2006; 53(3):98-108
-
Malamed SF. The periodontal ligament injection: an alternative to inferior alveolar nerve block. Oral Surg 1982; 53:117
-
Brandt R, Anderson P, Mc Donald N, Sohn W, Peters M. The pulpal anaesthetic efficacy of articaine versus lidocaine in dentistry. J Am Dent Assoc 2011; 142(5):493-504
-
Yapp K, Hopcraft M, Parashos P. Articaine: a review of the literature. Br Dent J 2011; 210:323-329
-
Srinivasan N, Kavitha M, Longanathan C, Padmini G. Comparison of the efficacy of 4% articaine and 2% lidocaine for maxillary buccal infiltrations in patients with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 133-136
-
Claffey E, Reader A, Nusstien J, Beck M, Weaver J. Anaesthetic efficacy of articaine for inferior alveolar blocks in patients with irreversible pulpitis. J Endod 2004; 30:568-571
-
Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine buccal infiltration enhances the effectiveness of lidocaine inferior alveolar nerve block. Int Endod J 2009; 42: 238-246
-
Moore PA, Boynes SG, Hersh EV, De Rossi SS, Sollecito TP, Goodson JM, Leonel JS, Flores C, Peterson C, Hutcheson M. The anesthetic efficacy of 4% articaine 1:200,000 epinephrine: two controlled clinical trials. J Am Dent Assoc 2006; 137:1,572-1,581
-
Septodont Inc Septocaine(articaine hydrochloride 4% with epinephrine 1,100,000) injection prescribing formulation. Manufacturer’s Drug Information Leaflet.
-
Jung IY, Kim JH, Kim ES, Lee CY, Lee SJ. An evaluation of buccal infiltrations and inferior alveolar nerve blocks in pulpal anesthesia for mandibular first molars. J Endod 2008; 34: 11-13
-
Corbett IP, Kanaa MD, Whitworth JM, meechan JG. Articaine infiltration for anesthesia of mandibular first molars. J Endod 2008; 34: 514-518
-
Garisto GA, Gaffen AS, Lawrence HP, Tenenbaum HC, Haas DA. Occurrence of paresthesia after dental local anesthetic administration in the United States. J Am Dent Assoc. 2010; 141:836-844
-
Hillerup S, Jensen RH, Ersboll BK. Trigeminal nerve injury associated with injection of local anesthetics: needle lesion of neurotoxicity. J Am Dent Assoc. 2011;142:531-539
-
Robertson D, Nusstein J, Reader A, Beck M, Mc Cartney M. The anesthetic efficacy of articaine in buccal infiltration of mandibular posterior teeth. J Am Dent Assoc. 2007; 138:1104-1112
-
Haas DA, Lennon D. A 21 year retrospective study of reports of paresthesia following local anesthetic administration. J Can Dent Assoc 1995;61:319-330
-
Werdehausen WR, Fazeli S, Braun S, Hermanns H, Essman F, Hollman MW, Bauer I, Stevens MF. Apoptosis induction by different local anaesthetics in a neuroblastoma cell line. Br J Anaesth 2009; 103: 711-718
-
Haas DA. Localized complications from local anesthesia. J Calif Dent Assoc 1998; 26:677-682
-
Hartnell NR, Wilson JP. Replication of the Weber effect using postmarketing adverse event reports voluntarily submitted to the United States Food and Drug Administration. Pharmacotherapy 2004; 24:743-749
-
Pogrel MA, Schmidt BL, Sambajon V, Jordan RC. Lingual nerve damage due to inferior alveolar nerve blocks: a possible explanation. J Am Dent Assoc 2003; 134: 195-199
-
Stacey GC, Hajjar G. Barbed needle and inexplicable paraesthesias and trismus after dental regional anaesthesia. Oral Surg Oral Med Oral Pathol 1994; 77:585-588
-
Penarrocha-Diago M, Sanchis- Bielsa JM. Opthalmologic complications after intraoral local anesthesia with articaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90:21-24
-
Malanin K, Kalimo K. Hypersensitivity to the local anesthetic articaine hydrochloride. Anesth Prog 1995; 42:144-145
-
Torrente-Castells E, Gargallo- Albiol J, Rodriguez- Baeza A, Berini-Aytes L, Gay- Escoda C. Necrosis of the skin of the chin: a possible complication of inferior alveolar nerve block injection. J Am Dent Assoc 2008; 139:1,625-1,630
-
Elad S, Admon D, Kedmi M, Naveh E, Benzki E, Ayalon S, Tuchband A, Lutan H, Kaufman E. The cardiovascular effect of local anesthesia with Articaine plus 1:200,000 adrenaline versus Lidocaine plus 1:100,000 adrenalin in medically compromised cardiac patients: a prospective randomized double blinded study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105:725 -730
-
Oertel R, Rahn R, Kirch W. Clinical pharmacokinetics of articaine. Clin Pharmacokinet 1997; 33; 417-425
-
Becker DE, Reed KL. Local Anesthetics: Review of Pharmacological Considerations. Anesth Prog. 2012 Summer; 59(2): 90-102
-
Westfall TC, Westfall DP. Adrenergic agonists and antagonists. In: Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York, NY: Mc Graw-Hill Companies Inc; 2011
-
Dionne RA, Goldstein DS, Wirdzek PR. Effects of diazepam premedication and epinephrine-containing local anesthetic on cardiovascular and catecholamine responses to oral surgery. Anesth Analg. 1984; 63:640-646
-
Hersh EV, Giannakopoulos H, Levin LM et al. The pharmacokinetics and cardiovascular effects of high-dose articaine with 1:100,000 and 1:200,000 epinephrine. J Am Dent Assoc. 2006;137:1562-1571
-
Schecter E, Wilson MF and Kong, YS, Physiologic responses to epinephrine infusion: the basis for a new stress test for coronary artery disease. Am Heart J 105:554-60, 1983
-
Dimsdale JE, Moss J. Plasma catecholamines in stress and exercise. J Am Med Assoc 1980; 243:340-2
-
Gandy W. Severe epinephrine-propranolol interaction. Ann Emer Med. 1989;18:98-99
-
Malamed SF, Handbook of Dental Anesthesia, Elsevier Mosby, St Louis Mo, USA, 5th edition, 2004
-
Doman S. An audit of the use of intra-septal local anesthesia in a dental practice in the South of England. Prim Dent Care 2011; 18: 143-147
-
Godzieba A, Smektala, Jedrzejewski M, Sporniak-Tutak K. Clinical Assessment of the safe use local anaesthesia with vasoconstrictor agents in cardiovascular compromised patients: A systematic review. Med Sci Monit. 2014; 20: 393-398
-
Tallman RD, Rosenblatt RM, Weaver JM, Wang YL. Verapamil increases the toxicity of local anesthetics. J. Clin Pharmacol 1988 Apr; 28(4): 317-21
-
Adsan H, Tulunay M, Onaran O. The effects of verapamil and nimodipine on bupivacaine-induced cardiotoxicity in rats: as in vivo and in vitro study. Anesth Anal 1998 April; 86(4): 818-24
-
Becker DE. Adverse drug interactions. Anesth Prog. 2011; 58:31-41
-
Foster CA, Aston SJ. Propranolol-epinephrine interaction: a potential disaster. Plast Reconstr Surg. 1983; 72: 74-78
-
Struthers AD, Reid JL, Whitesmith R, Rodger JC. Effect of intravenous adrenaline on electrocardiogram, blood pressure and serum potassium. Br Heart J 1982; 49: 90-93
-
Meechan JG, Rawlins MD. The effect of adrenaline in lignocaine anaesthetic solutions on plasma potassium in healthy volunteers. Eur J Clin Pharmacol 1987; 32: 81-83
-
Mimram A, Ribstein J, Sissman J. Effects of calcium channel blockers on adrenaline- induced hypokalaemia. Drugs 1993; 46(Suppl 2): 103-107
-
Peruse R, Goulet JP, Turcotte JY. Contraindications to vasoconstrictors in dentistry: Part 1, cardiovascular diseases. Oral Surg Oral Med Oral Pathol 1992, 74:679-86
-
Little JW, Falace DA et al. Dental Management of the Medically Compromised Patients, 5th ed. Mosby – Year Book, St Louis, 1997
-
Becker DC, Drug interactions in dental practice: a summary of facts and controversies. Compend Cont Educ Dent 1994, 15:1228-44
-
Muzyka BC. Atrial fibrillation and its relationship to dental care. J Am Dent Assoc 1999, 130: 1080-5
-
United States Department of Health and Human Services: Warning on Prescription Drugs Containing Sulfites, FDA Drug Bull, 17: 2-3, 1987
-
Seng GF, Gay BJ. Dangers of sulfites in dental local anesthetic solutions: warning and recommendations. J Am Dent Assoc 1986, 113: 769-70
-
Bush RK, Taylor SL et al. Prevalence of sensitivity agents in asthmatic patients. Am J Med 1986, 81:816-20
-
Perusse R, Goulet JP, Turcotte JY. Contraindications to vasoconstrictors in dentistry: Part II, hyperthyroidism, diabetes, sulfite sensitivity,cortico-dependent asthma and pheochromocytoma. O Surg O Med O Path 1992, 74: 687-91
-
Demas PN, JR Mc Clain. Hepatitis: implications for dental care. Oral Surg Oral Med Oral Pathol 88(1):2-4, 1999
-
Yagiela JA. Adverse drug interactions in dental practice: interactions associated with vasoconstrictors. J Am Dent Assoc 1999, 130:701-9
-
Goulet JP, Perusse R, Turcotte JY. Contraindications to vasoconstrictors in dentistry: Part III, pharmacologic interactions. Oral Surg Oral Med Oral Pathol 1992 74:692-7
-
Greenwood I, Heylen R, Zakrzewska JM. Anti-retroviral drugs – implications for dental prescribing. Br Dent J 1998; 184:478-482
-
Friedlander AH, Mahler M, Norman KM, Ettinger RL. Parkinson disease: systemic and orofacial manifestations, medical and dental management. J Am Dent Assoc 2009 Jun; 140(6): 658-69
-
Moore PA, Hersh EV, Papas AS et al. Pharmacokinetics of lidocaine with epinephrine following local anesthesia reversal with phentolamine mesylate. Anesth Prog. 2008; 55:40-48
CPD responses closed
The CPD quiz for this article is now closed. Please check the listings for the current quizzeslistings

Comments are closed here.