Non-invasive facial aesthetics
A demonstration of the effectiveness of the Forma device for non-invasive skin tightening. The second part of this article will look at a case treatment step by step at the Scottish Centre for Excellence in Aesthetics
As we age, our collagen and elastic tissues degrade, resulting in excess, loose skin; this is often one of the first signs of facial ageing. As a result, surgical rhytidectomy (facelifts) remains a common surgical procedure to help reverse this ageing process, with 133,320 facelift procedures performed in 2013, the most recent year for which data is available from the American Society of Plastic Surgeons 1. While facelifts remain an extremely effective method to reduce static rhytids, there has been a dramatic paradigm shift toward non-surgical skin tightening and rejuvenation techniques, as patients seek to achieve skin tightening with no or minimal downtime procedures.
In 2013, 293,388 non-surgical skin tightening procedures and 456,613 photo-rejuvenation procedures were performed, a much higher volume than traditional surgical facelifts, according to the American Society for Aesthetic Plastic Surgery 2.
While many technologies including infrared lasers, intense pulsed light devices, and resurfacing lasers have been utilised to heat the deep dermis, thereby resulting in skin tightening, the results have typically been modest 3–5. Recently, intense focused ultrasound has been proposed as a potential option for skin tightening; however, these treatments are associated with pain and downtime 6. An ideal skin tightening treatment would be efficacious, pain free, require no anaesthesia, and result in no downtime.
Radiofrequency (RF) technology represents a potentially promising option for non-invasive skin tightening to achieve these ideals. RF devices utilise electrical conductance, in the form of rapidly alternating electrical current (various frequencies can be utilised, but they are typically greater than 1,000,000 cycles per second), to cause oscillation of cellular structures that are in the electrical path, thereby increasing intermolecular motion. As the current flows alternatively, molecular collisions increase, thereby creating thermal energy (heat). Thus, RF technology utilises the impedance (resistance) of tissue to generate heat rather than directly transferring heat.
Historically, the majority of RF devices were monopolar devices; however, these initial devices had relatively limited efficacy in skin tightening and could be associated with pain, burns, or other adverse effects 7,8. More recently, bipolar RF devices, incorporating both positive and negative electrodes, have been developed with potentially greater efficacy and an improved safety profile due to the creation of a closed electrical circuit. The depth to which the current penetrates is a function of the distance between the positive and negative electrodes; greater distance between the bipolar terminals results in greater depth of energy penetration.
The controlled heat exposure from bipolar RF devices can be directed to the dermis of the tissue, causing controlled dermal heating of collagen, while sparing the epidermis. As the dermis is heated, the triple helical shape of collagen is broken due to disruption of the intramolecular heat-labile bonds connecting the helices, while the heat-stable intermolecular bonds are unaffected. These effects allow the triple helix to unravel and shorten, resulting in tighter, more compact collagen9.
Ultimately, dermal heating results in collagen stimulation and neocollagenesis10. The heating of collagen can be modelled by the principles of the Arrhenius equation, indicating that the reaction rate of heating collagen is dependent both on time and temperature 11,12. If high dermal temperatures are achieved, low exposure times are necessary. At a temperature of 85°C, an exposure time of ˜1 ms is enough to induce structural changes to collagen13.
Historically, static (or stamping) RF devices utilised relatively higher peak temperatures with low exposure times; however, high peak temperatures also increase the risk of burns and other adverse events. Alternatively, according to the Arrhenius equation, lower peak temperatures could be utilised to reduce the risk of side effects, but this would require longer exposure periods in order to effectively remodel collagen. As an example, at a temperature of 43°C, an exposure time ranging from ˜90 seconds to 5 minutes is necessary to induce collagen remodelling. Recently, novel dynamic (or moving) RF devices have been developed, which utilise lower peak temperatures with longer exposure times; these devices require that the handpiece is moved across the skin surface during the treatment to sustain the dermal matrix at an elevated temperature.
Historically, RF devices had difficulty in uniformly achieving and maintaining these constant temperatures for several minutes to effectively remodel collagen, thereby limiting the effectiveness of these dynamic RF devices 14.
Equipment
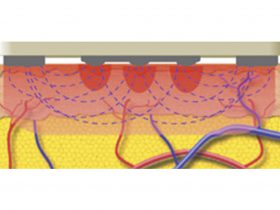
Forma (InMode Inc, Richmond Hill, ON, Canada, North America) is an FDA-approved, bipolar, noninvasive RF device that generates controlled dermal heating. The device incorporates multiple novel technologies to allow for prolonged, controlled dermal heating while limiting the potential for side effects. The device handpiece incorporates two central rows of seven smooth RF-emitting positive electrodes (14 polar) with current flowing from the positive electrodes to the two negative side electrode bars (Figure 2). The RF current travels to a maximum depth of half the distance between the electrodes and is thus confined to the dermis, creating a uniform dermal heating pattern (Figure 3).
The device also allows the treating physician to determine and set the optimal dermal temperatures (in Celsius) to be maintained throughout the treatment, as well as the energy delivered via the handpiece (in millijoules). In order to achieve and maintain this temperature, the device handpiece incorporates several sensors, including high and low impedance sensors, a contact sensor, and an epidermal thermal sensor. The device measures skin temperature, impedance, and epidermal contact 10 times per second allowing for real-time feedback.
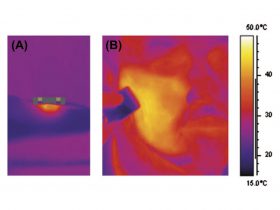
When the treatment area reaches the predetermined temperature, or if the tissue impedance drops quickly or contact is broken, the device immediately, automatically, and temporarily terminates the delivery of RF energy to this area. Once the temperature of this treatment area drops to 0.1°C below the set target temperature, or as the physician moves the treatment applicator over a new area, which has not yet reached the predetermined temperature, the device automatically reactivates the RF energy. This real-time immediate feedback allows for the physician to achieve, control, and extend the thermal treatment while limiting the potential for adverse effects. As a result, the physician is able to safely, comfortably, and effectively achieve uniform heating of large treatment areas (Figure 4), while minimising pain and the potential for burns or other adverse effects.
Discussion
Non-invasive skin tightening represents a rapidly emerging area in cosmetics, as patients increasingly seek to avoid facelifts and other invasive procedures. Non-ablative heating of the dermis and subcutaneous tissue offers the potential for skin tightening and rhytid reduction with minimal pain, downtime, and low risk of scars or other adverse events. Multiple non-invasive technologies including intense pulsed light, lasers, RF, and ultrasound have been studied as therapeutic options; however, the clinical efficacy of these modalities has been limited and difficult to reproduce on a consistent basis. Additionally, several devices, such as focused ultrasound, have been associated with significant pain and/or downtime.
The bipolar RF device mentioned in this article is a novel, safe, and effective technology for inducing skin tightening. In a study, of 14 patients conducted by the authors 15, all treated patients were determined to have an effective treatment resulting in skin tightening and rhytid reduction following a series of four to six-weekly RF treatments; over 70 per cent of treated patients were observed to have a moderate or significant clinical improvement. This represents an extremely high response rate, as well as significant level of improvement not seen with previous RF and other non-invasive skin-tightening technologies.
This RF device offers several advantages over currently available technologies, which likely explains this high level of clinical efficacy. The Forma device utilises real-time temperature-monitoring mechanisms, assessed by measuring tissue impedance, temperature, and epidermal contact throughout the treatment. This allows the device to continuously monitor the targeted tissue, and adjust the delivery of the RF energy to create a uniform heating exposure. The device is also able to maintain this constant uniform heating exposure for prolonged periods over relatively large treatment areas, such as an entire unilateral cheek. This uniform, long exposure is likely more effective at inducing collagen remodelling and neocollagenesis. Additionally, since the thermal exposure can be extended and prolonged, lower temperatures that do not induce any pain can be utilised.
Rather than applying high, painful temperatures for seconds, this device allows for controlled, comfortable dermal heating to be maintained for several minutes to induce collagen tightening and remodelling. The use of lower temperatures over a longer exposure period allows for the treatment to be pain free with no downtime. In contrast to many other devices, when using the device under investigation, none of the subjects in our study required any anaesthesia, including topical, and none required stopping the treatment or reducing the treatment parameters. Thus, this device represents a safe and effective non-invasive option for facial skin tightening.
Our study, of course, has its limitations. Face tightening, particularly of the lower face, is difficult to assess with quantifiable measures. There are no fixed anatomic structures that lend themselves well to measurement on the lower face to determine lift or tightening effects. As a result, we utilised randomised photographic comparisons in this study, similar to other peer-reviewed skin tightening clinical studies. In the future, perhaps it will be possible to develop and validate more objective measures for lower face tightening and rhytid reduction. This study was also conducted in a single centre, with a female study population; this may impact the generalisability of the data to larger, more diverse populations. Finally, the long-term impact of the treatments on skin tightening over the course of years is not yet known.
- FIGURE 1: The Forma device in use
- FIGURE 2: RF handpiece with two central rows of seven smooth RF-emitting positive electrodes (14 polar) with current flowing from the positive electrodes to the two negative side electrodes.
- FIGURE 3: Representation of alternating current flowing between the positive (central) electrodes and negative (side) return plates
- FIGURE 4: In vivo thermal view showing the initial application of Forma handpiece (A) and following treatment, a uniform heat distribution at 43°C across an entire right cheek (B).
More info
To find out more about the Scottish Centre for Excellence in Aesthetics, phone 0141 427 4530, email enquiry@scottishdentistry.com or visit www.scottishaesthetics.com
References
- American Society of Plastic Surgery. Available from: www.plasticsurgery.org/Documents/news-resources/statistics/2013-statistics/cosmetic-procedures-nationaltrends-2013.pdf [cited 2015 January 23].
- Moretti M. Skin tightening: Softening demand in a weak economy. Medical Insight Inc; 2008.
- Dierickx C C. T he role of deep heating for noninvasive skin rejuvenation. Lasers Surg Med. 2006; 38: 799-807.
- Goldberg D J. Nonablative dermal remodeling: Does it really work? Arch Dermatol. 2002; 138: 1366-1368.
- Sadick NS. Update on non-ablative light therapy for rejuvenation: A review. Lasers Surg Med. 2003; 32: 120-128.
- Chan NP, Shek SY, Yu CS, Ho SG, Yeung CK, Chan HH. Safety study of transcutaneous focused ultrasound for non-invasive skin tightening in Asians. Lasers Surg Med. 2011; 43: 366-375.
- Weiss RA, Weiss MA, Munavalli G, Beasley KL. Monopolar radiofrequency facial tightening: A retrospective analysis of efficacy and safety in over 600 treatments. J Drugs Dermatol. 2006; 5: 707-712.
- Abraham MT, Mashkevich G. Monopolar radiofrequency skin tightening. Facial Plast Surg Clin North Am. 2007;15: 169-177.
- Zelickson B D, Kist D, Bernstein E, Brown D B, Ksenzenko S, Burns J, et al. Histological and ultrastructural evaluation of the effects of a radiofrequency-based nonablative dermal remodeling device: A pilot study. Arch Dermatol. 2004; 140: 204-209.
- Alster TS, Lupton JR. Nonablative cutaneous remodeling using radio frequency devices. Clin Dermatol. 2007; 25: 487-491.
- Akeson WH. Application of the Arrhenius equation to rat tail tendon collagen. Nature. 1963; 199: 185-186.
- Ross E V, Yashar S S, Naseef G S, Barnette D J, Skrobal M, Grevelink J, Anderson RR. A pilot study of in vivo immediate tissue contraction with CO2 skin laser resurfacing in a live farm pig. Dermatol Surg. 1999; 25: 851-856.13. Sadick N. Tissue tightening technologies: Fact or fiction. Aesthet Surg J. 2008; 28: 180-188.
- Harth Y, Lischinsky D. A novel method for real-time skin impedance measurement during radiofrequency skin tightening treatments. J Cosmet Dermatol. 2011; 10: 24-29.
- Nelson A, Beynet D, Lask GP. A novel non-invasive radiofrequency dermal heating device for skin tightening of the face and neck. J Cosmet Laser Ther. Vol. 17, Iss. 6, 2015.



Comments are closed here.