Dental Antibiotics: Curbing Over-Prescribing
Scottish group aims to engage with the profession and organisations to reduce levels
The topic of antimicrobial resistance (AMR) is one which has become increasingly important over recent years as the development of resistance continues to outstrip the rate of new antimicrobial drug development.
Over the last few years, we have seen the emergence of an increasingly broad spectrum of pathogens becoming more resistant to a dwindling supply of new antibiotics. Examples include oral mucositis caused by Methicillin resistant Staphylococcus Aureus (MRSA) and the emergence of vancomycin resistant enterococci (VRE) – linked to endodontic infections1,2.
These examples from maxillo-facial infections are the tip of an iceberg in comparison to medical antimicrobial resistance and are underlined by the personal tragedies for those who become infected by them. There are now many initiatives aimed at addressing this ‘silent pandemic’ including the annual WHO World AMR awareness week held annually in November as well as campaigns in the UK such as the Antibiotic Guardian programme and the ‘antibiotics don’t cure tooth ache’ message.
The dental subgroup of the Scottish Antimicrobial Prescribing Group (SAPG-Dental) has an antimicrobial stewardship (AMS) focus ranging from working with partners to promote oral health and reduce infections, optimising selection of first choice antimicrobials and monitoring antimicrobial use in dentistry.
A key finding from the SAPG-Dental group has been the observation that antibiotic prescribing by General Dental Practitioners (GDPs) in Scotland declined by 17.7% between 2015 and 20193, which was a testament to the success of previous educational campaigns and antimicrobial stewardship of the dental profession.
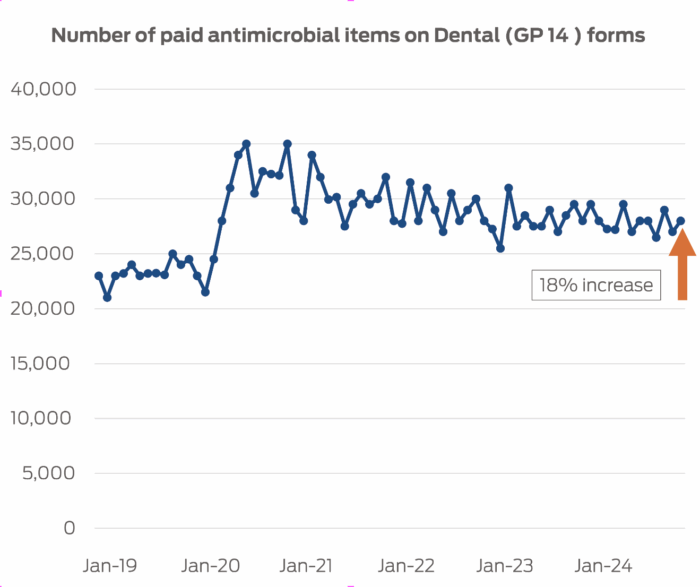
Unfortunately, during the pandemic several backward steps were taken in antimicrobial stewardship terms by reversing the ‘antibiotics don’t cure toothache’ evidence with the triple A (Advice, Analgesia & Antibiotics) recommendation from Government sources for managing acute dento-alveolar infections. This resulted in a significant increase in antibiotic prescribing between April 2019 and April 2020 with monthly prescriptions rising to a peak of 35,000 items per month compared with around 23,000 items per month prior to the pandemic.
The advice to routinely prescribe antibiotics for all dental infections undermined previous evidence and policies that antibiotics do not cure toothache. Since the pandemic however, the pre-COVID decline in antibiotic prescribing has reversed, antibiotics prescribing has increased, and levels remain at approximately 20% higher than before the pandemic (Figure 1).
To understand more about this issue, and to propose solutions, the Scottish Antimicrobial Prescribing Group (SAPG) Committee tasked the SAPG Dental Stewardship Steering Group (DSSG) with understanding the driving factors linked to this increase in prescribing.
To achieve this, a Short Life Working Group (SLWG) was set up by DSSG that had representation from area dental committees, dental practice advisors, Directors of Dentistry, the University of Glasgow Dental School, Chief Dental Office (CDO), Public Health Scotland (PHS), NHS Education for Scotland (NES), dental practitioners in primary and secondary care and SAPG and ARHAI Scotland.
THE SLWG reviewed outputs from a wide range of data sources that included rates of antibiotic prescribing by general dental practitioners (GDPs), dental treatment claims, NHS24 calls, NHS board waiting times, questionnaire data on GDPs on attitudes towards prescribing and rates of hospital admissions for dento-alveolar infections. This data was analysed and discussed with representative experts at the SLWG.
The SLWG concluded that the delayed return of antibiotic prescribing in general dental practice post-pandemic is due to multiple factors that range from changes in prescribing policy during the pandemic, increasing difficulties in accessing dental care in the post-pandemic period and changes in patient expectations with respect to antibiotic prescribing.
| Recommendations of the DSSG Short Life Working Group |
|---|
| To raise awareness within dental organisations and wider Government of the impact of systems pressures for dental treatment access and impact on dental prescribing. |
| Continue to monitor and report dental antibiotic prescribing and the impact of the new renumeration process Determination 1. |
| Improve communications to GDPs on the excess of antibiotic prescribing through relevant organisations such as, NES, the office of the Chief Dental Officer and Directors of Dentistry. |
| Conduct further research to understand the root causes and in particular explore the impact of social deprivation and access to dental care on both prescribing and dental complications. |
| Review and commission education initiatives for antimicrobial stewardship aimed at both GDPs and patients. |
| Apply lessons learned from the last pandemic into Pandemic preparedness plans to ensure that there is appropriate access for patients with acute dental infections to dental surgical services. |
The aim of this paper is to ensure that the dental profession in Scotland is aware of this increase in antibiotic prescribing and provide a summary of the conclusion and recommendations of the work of the SLWG (Table 1). SAPG-Dental are keen to engage with the profession and dental organisations to work together to reduce overall antimicrobial prescribing in dentistry in Scotland over the coming months and years to come.
- Smith AJ, Robertson D, Tang MK, Jackson MS, MacKenzie D,
Bagg J. Staphylococcus aureus in the oral cavity: a three-year retrospective analysis of clinical laboratory data. Br Dent J. 2003 Dec 20;195(12):701-3; discussion 694. doi: 10.1038/sj.bdj.4810832. PMID: 14718964. ↩︎ - Rusinovci S, Sejdini M, Salihu S, Haliti N, Juki DP, Starc A, Stubljar D, Jukic T. Commensal mouth bacteria are the main cause of dentoalveolar abscesses in the maxillofacial region. J Infect Dev Ctries. 2025 Jan 31;19(1):107-116. doi: 10.3855/jidc.20202. PMID: 39977474. ↩︎


Comments are closed here.