Silver service dentistry
While not a new practice, the evidence shows that the use of silver diamine fluoride is safe and effective in the prevention and treatment of dental caries
The use of silver-based compounds as antimicrobial agents has been well-documented and common practice for more than 100 years in both medicine and dentistry. From wound dressings to water purification systems, Ag+ is able to destroy pathogens at concentrations of <50ppm. More recently, the use of silver diamine fluoride (SDF) in dentistry has been increasing with applications including caries prevention, arresting carious lesions and the treatment of sensitivity 1.
There are a vast number of products that have been used to deliver fluoride in the aim of preventing caries including milk, salt, toothpaste and varnish. It is thought that where SDF differs is that the silver salt component has a potent antibacterial effect with the ability to encourage the formation of calcified/sclerotic dentine while the fluoride provides a remineralising effect. As such, SDF has stimulated significant interest in the prevention and treatment of caries worldwide based on its ability to reduce instances of pain, ease of use, affordability, non-invasive nature and minimal clinical time for application 1.
SDF is a colourless topical agent with a large number of practical clinical applications in dentistry including 2:
1) Prevention and treatment of high caries risk patients including both children and adults.
2) Prevention and treatment of caries in patients who are medically compromised.
3) Treatment of root surface caries.
4) Treatment of dentine hypersensitivity.
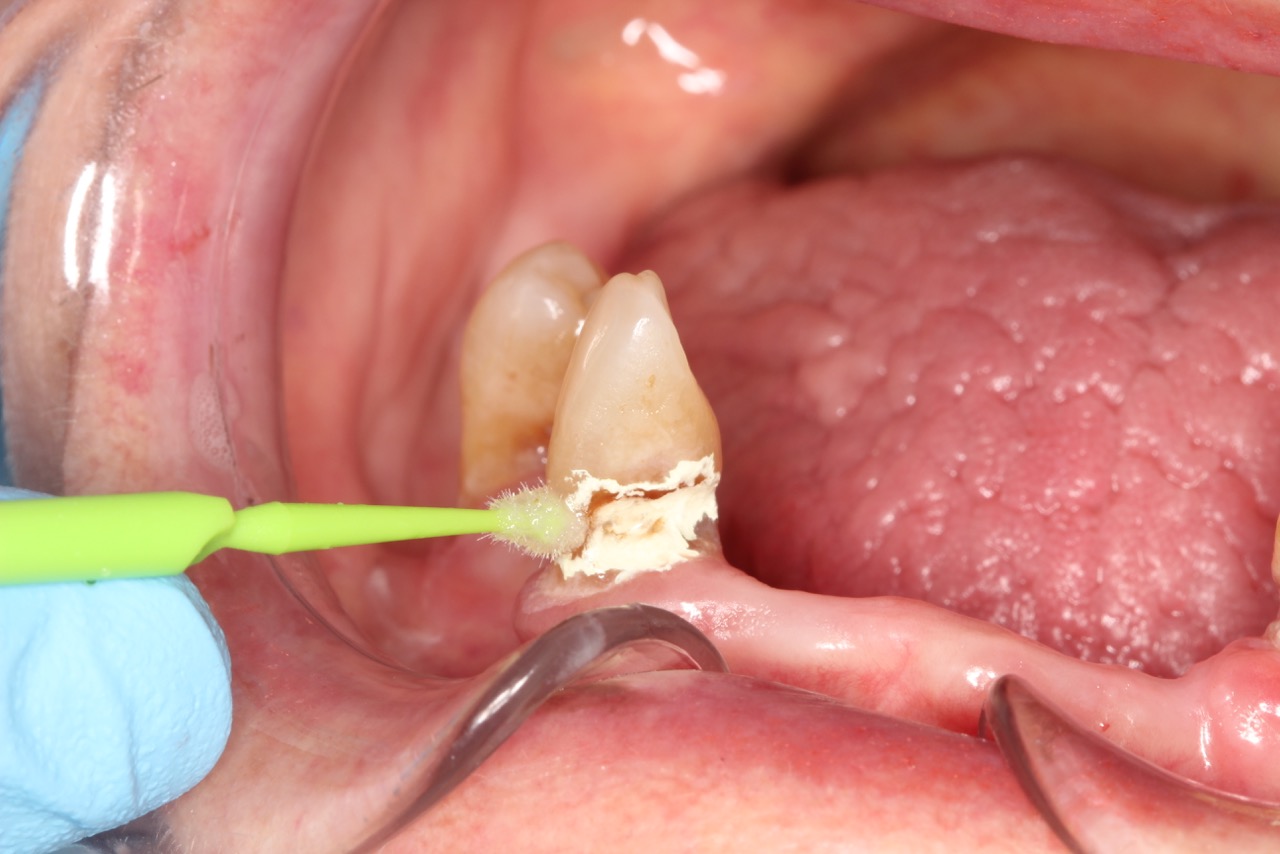
SDF is commercially available in the UK as Riva Star by SDI. The formulation is based on two coloured capsules, silver and green, that must both be applied. Application of SDF is a relatively simple process. The teeth must be cleaned with prophy paste to remove plaque debris before being dried and isolated with cotton wool rolls. If applying close to the gingival margin the kit contains a gingival barrier or alternatively some Vaseline can be placed. The silver capsule is applied first followed by green that causes the formation of a white precipitate. Each capsule can be used to treat around five teeth (see Figs 1-3).
Where being used in the treatment of caries it is important that patients are aware that the aim is to arrest the lesion that will result in a dark appearance (Fig 3). Temporary staining of the gingivae is also possible. Repeated application, twice annually, is essential where the aim is to arrest a carious lesion or to treat dentine hypersensitivity.
- Figure 1. Root surface caries
- Figure 2. Application of Riva Star silver fluoride
- Figure 3. Application of Riva Star potassium iodide
- Figure 4. Post-treatment root surface
- Figure 5. Post-treatment deciduous molar tooth
Caries prevention
A systematic review by Rosenblatt et al. conducted a review of the literature on the use of SDF between 1966 and 2006, identifying 99 papers. The authors were able to conclude that SDF is more effective than fluoride varnish and may be a valuable preventative intervention. They also noted that SDF is a “safe, effective, efficient and equitable caries preventive agent that meets the criteria of the WHO millennium goals”1.
In 2017, a further review of the literature conducted by Contreras et al. found 33 publications meeting the inclusion criteria that were published between 2005 and 2016. The group were able to conclude that SDF is an “effective preventative treatment in a community setting” and that is “shows potential to arrest caries in the primary dentition and permanent first molars”3.
Caries treatment
Chu et al. carried out a study on the use of SDF in arresting carious lesions in 370 Chinese pre-school children aged three to five years old. They compared groups of children receiving SDF treatment, sodium fluoride varnish and a control. The children were followed up for 30 months receiving an intervention every three months.
Children in the SDF groups had a mean of 2.8 arrested lesions compared with a mean of 1.5 in the varnish group. They were able to conclude that the application of an SDF solution was more effective in arresting dentine caries in primary teeth compared with sodium fluoride vanish 4.
Similar results are echoed in a study by Lo et al. which followed 375 Chinese pre-school children over an 18-month period comparing groups of children receiving treatment with SDF, NaF varnish and a control. They found a mean of 0.4 new carious lesions in the SDF treated group compared with 1.2 in the control. They also found similar results in arresting active carious lesions with a mean of 2.8 arrested lesions in the SDF group compared to 1.5 in the NaF varnish group 5.
Clemens et al. treated 118 active lesions with SDF in a community dental clinic in Oregon. They were able to follow up 102 lesions on a three-monthly recall basis and found that 100 lesions were arrested by the first recall and all lesions by the second recall. The authors also noted no incidence of pain or infection and that the parents had a favourable view of the treatment modality 6.
Adults patients have also found a beneficial effect from SDF treatment. Zhang et al. followed up 227 elderly patients over 24 months who were provided with SDF and oral health education compared with a control group. They found a statistically significant result in that the SDF group had fewer root surface lesions than the control group. The authors concluded that SDF combined with oral health education was effective in preventing new root caries and arresting existing lesions in elderly patients 7.
Treatment of sensitivity
Castillo et al carried out a randomised control trial in 126 adult patients experiencing dentine hypersensitivity to assess the effectiveness of SDF as a desensitising agent. They found a reduction in sensitivity at seven days that was statistically significant (p<0.001) compared with the control group and were able to conclude that SDF is a clinically effective desensitising treatment 8.
Guidelines
In October 2017, the American Academy of Paediatric Dentistry issued the first ever evidence-based guideline for the use of SDF in the treatment of dental caries. This followed a systematic review of research between 1969 and 2016. The guideline hopes to lead to a more widespread adoption of SDF as a treatment for dental caries in paediatric and special needs patients 9.
The AAPD describe SDF as the “single greatest innovation in paediatric dental health in the last century aside from water fluoridation” noting the cost effective and pain-free benefits of treatment.
The systematic review on which the guideline is based notes no adverse effects but that a ‘downside’ is the black appearance of cavities. The potential to reduce the number of paediatric cases requiring sedation or GA is high.
The chairside guide suggests that patients who may benefit from SDF include 10:
- High caries risk individuals with active cavitated carious lesions in anterior or posterior teeth
- Patients with additional behavioural or medical challenges who present with cavitated carious lesions
- Multiple cavitated lesions that may not all be treated in a single visit
- Patients with limited access to dental care.
- The chairside guide also suggests the following criteria for tooth selection 9:
- No clinical signs of pulpal inflammation or reports of spontaneous pain
- Cavitated lesions not encroaching on pulp
- Lesions are accessible by a brush to apply SDF (orthodontic separators may be used to help gain access to interproximal regions).
Follow-up is recommended two to four weeks after treatment. Arrested lesions can subsequently be restored. However, where lesions are not restored, biannual re-application is recommended.
In conclusion, silver diamine fluoride is safe and effective in the prevention and treatment of dental caries as well as providing a further treatment modality in the management of dentine hypersensitivity. Application twice annually is a minimally invasive, cost-effective treatment that demonstrates a potentially vast benefit to patients of all ages.
References
1. Rosenblatt A, Stamford T and Niederman R. (2009). Silver Diamine Fluoride: A Caries “Silver-Fluoride Bullet”. Journal of Dental Research, 88(2), pp.116-125.
2. JUCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc. 2016 Jan; 44(1): 16–28.
3. Contreras et al. 2017. Effectiveness of silver diamine fluoride in caries prevention and arrest: a systematic literature review Gen Dent. 2017 May-Jun; 65(3): 22–29..
4. Chu C, Lo E and Lin H. (2002). Effectiveness of Silver Diamine Fluoride and Sodium Fluoride Varnish in Arresting Dentin Caries in Chinese Pre-school Children. Journal of Dental Research, 81(11), pp.767-770.
5. Lo E, Chu C and Lin H. (2001). A Community-based Caries Control Program for Pre-school Children Using Topical Fluorides: 18-month Results. Journal of Dental Research, 80(12), pp.2071-2074.
6. Clemens J, Gold J and Chaffin J. (2017). Effect and acceptance of silver diamine fluoride treatment on dental caries in primary teeth. Journal of Public Health Dentistry.
7. Chu C, Lo E and Lin H. (2002). Effectiveness of Silver Diamine Fluoride and Sodium Fluoride Varnish in Arresting Dentin Caries in Chinese Pre-school Children. Journal of Dental Research, 81(11), pp.767-770.
8. Castillo J, Rivera S, Aparicio T, Lazo R, Aw T, Mancl L and Milgrom P. (2010). The Short-term Effects of Diammine Silver Fluoride on Tooth Sensitivity. Journal of Dental Research, 90(2), pp.203-208.
9. Chairside Guide: Silver Diamine Fluoride in the Management of Dental Caries Lesions. AAPD Reference Manual v 39. No.6, 17/18. Accessed on http://bit.ly/AAPDchairsideguide
About the authors
Michael Dhesi is a GDP who qualified in 2012 with BDS(Hons) from the University of Glasgow and has subsequently completed MFDS RCPS(Glasg) and an MSc in Advanced General Dental Practice at the University of Birmingham. Michael’s focus is in minimally invasive and adhesive restorative dentistry. He also has interests in the management of dental anxiety and oral surgery.
Clive Schmulian qualified from Glasgow University in 1993. Throughout his time in general dental practice, he has developed his clinical skills by obtaining a range of postgraduate qualifications, which in turn led him to develop an interest in digital imaging in both surgical and restorative dentistry. He is a director of Clyde Munro.
CPD responses closed
The CPD quiz for this article is now closed. Please check the listings for the current quizzeslistings






Comments are closed here.