Management of the open apex in endodontics
Current techniques and new solutions when dealing with the open apex in root canal surgery
The anatomy of the apical foramen changes with age as root formation has yet to be completed when teeth erupt. The completion of root development and closure of the apex occurs up to three years after eruption1.
Patients who present with immature apical formation (see Fig 1) pose a challenge due to the presence of large open apices along with divergent and thin dentinal walls that are susceptible to fracture. Historically, we have tried to generate formation of an apical barrier by repeated placement of calcium hydroxide over many months, or more recently by immediate barrier formation with a Mineral Trioxide Aggregate (MTA) plug.
Ideal management would involve regeneration of new pulpal tissue and continued root formation. Novel techniques for dealing with immature apices such as apexogenesis sometimes claim to be regenerative techniques. However, assessment of the composition of this regenerated tissue has proven to be difficult and it seems that it is made up of periodontal and bone tissue rather than tissue of pulpal origin2. As clinicians we need to consider whether this is better than formation of an apical barrier and obturation by conventional means?
Root development (see Table 1)
Classically, there are two types of open apices; blunderbuss and non-blunderbuss. In the former, the walls of the canal are divergent and flaring, the apex is funnel shaped and typically wider than the coronal aspect of the canal. In a non-blunderbuss apex, the walls of the canal may be parallel to slightly convergent. The apex, therefore can be broad shaped or convergent.
What are the causes of open apices?
Incomplete root development often arises secondary to pulpal necrosis arising as a result of caries or trauma. Both foraminal and peri-foraminal resorption of the root end may also arise in the presence of a periapical lesion4. This may alter the anatomy of a pre-existing open apex further. Iatrogenic enlargement of the root end may also arise due to poor control of working length and subsequent enlargement with both hand and rotary files.
What problems are faced clinically?
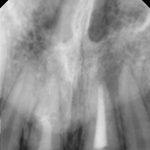
Teeth with open apices often tend to have thin dentinal walls that are susceptible to fracture before, during or after endodontic treatment. Frequently, they present with periapical lesions, which may or may not be associated with apical resorption. Short roots compromise the crown-root ratio, often affecting long-term prognosis.
Fractures of the crown are common following trauma. This can compromise aesthetics, especially in the anterior region, and there may be a lack of tooth tissue present. In long-standing cases these teeth may also undergo discolouration. Large open apices pose a challenge in determining the working length, decision on the necessity of root canal preparation, and achieving control
during obturation.
- Fig 1a
- Fig 1b
- Fig 1c
- Fig 1d
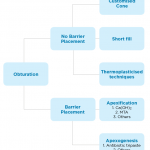
- Fig 2
- Fig 3
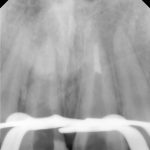
- Fig 4a
- Fig 4b
- Fig 4c
- Fig 4d
- Fig 4e
How is the working length determined?
There is relatively little data regarding the value of radiography and electronic apex locator (EAL) use when root formation is incomplete, and supplementary measurement techniques may be helpful. When using an EAL to measure working length in such cases, it is essential to use a file which is well matched to the apical size (see Fig 2) where possible. The paper point technique described by Rosenberg to supplement initial apex locator readings could be considered for the working length determination of open apices in relatively straight canals5.
Marcos-Arenal et al.6 in an in vivo study, demonstrated an 87 per cent accuracy of this technique in establishing working length to within 0.5mm of the apical foramen. While El Ayouti et al.7 proposed a tactile method involving the use of a size 25 K-file bent at the tip, with its orientation marked with a silicone ring. The file was bent to facilitate ease of use. In this study, 95 per cent of cases were accurate to within 0.5mm of the apical foramen.
Do I need to instrument the canal?
During conventional root canal treatment, the role of instrumentation is to achieve removal of vital and necrotic tissues from the root canal system, along with infected root dentine8. It aims to prepare the canal space to facilitate attempts at disinfection using irrigants and medicaments. As a result, minimal instrumentation of teeth with open apices (and thin dentinal walls) is needed due to the ease in placement of irrigation devices close to the working length.
How do I obturate the canal?
The options for obturation are dependent on whether or not we aim to create an apical barrier. Figure 3 highlights the different options. Apexification and apexogenesis are two endodontic procedures which attempt to either induce apical repair by initiating a hard tissue barrier across an open apex or to promote the continued formation of the apical portion of the root9.
Apexification
Calcium Hydroxide has been the first choice material for apexification. Placement and repeated changes over the course of five to 20 months induces the formation of a calcific barrier. The unpredictable and lengthy course of treatment presented challenges, particularly as it required a high level of patient compliance. For this reason, one visit apexification has been suggested.
MTA has been proposed as a material suitable for one visit apexification as it combines a bacteriostatic action, biocompatibility and a favourable sealing ability. Placement of a 3mm thickness of MTA in the apical portion of an ‘open apex’ permits the vertical condensation of warm gutta percha into the remainder of the canal (See Fig 4).
Apexogenesis
Case reports in the literature over the past 10 years have demonstrated successful revascularisation and regeneration of immature permanent teeth with apical periodontitis. Banchs and Trope10 irrigated necrotic teeth with sodium hypochlorite, and placed an antibiotic tri-paste dressing consisting of metronidazole, minocycline and ciprofloxacin. Four weeks later, the tooth was re-accessed and bleeding encouraged at the apex, allowing a clot to form 3mm below the CEJ. MTA was placed on the blood clot and the tooth restored with composite. Follow-up radiographs demonstrated complete apical healing and continued root formation.
Shin et al.11 treated a non-vital mandibular second premolar tooth using irrigation with 6 per cent sodium hypochlorite and 2 per cent chlorhexidine without instrumentation in a single visit. The successful outcome of this case report suggests that this conservative revascularisation treatment approach can create a suitable environment for pulpal repair, resulting in the completion of root maturation.
McCabe12 recently published a case report showing disinfection with 5 per cent sodium hypochlorite followed by the induction of a blood clot into the root canal space may be sufficient to promote revascularisation in certain circumstances using a single visit protocol.
Most of the case reports regarding apexogenesis as a treatment modality have shown an increase in dentinal wall thickening and root length, with a reduction in the volume of the pulp canal space visible radiographically. Histological analysis of teeth which had undergone revascularisation treatment demonstrated that the mineralised layer on the walls which was present appeared to be of periodontal origin rather than pulpal origin12.
What does the future hold?
It appears that current treatment approaches tend to stimulate reparative rather than regenerative responses in respect of the new tissue generated, which often does not closely resemble the physiological structure of dentine-pulp complex. Although patients requiring treatment undoubtedly make up a small proportion of our patients, and despite the biological limitations, such techniques appear to offer significant promise for improved treatment outcomes2.
The main question is whether our patients are better served by apexification and formation of an apical barrier via an MTA plug, or whether apexogenesis and generation of reparative tissue within the canal space, even if it is periodontal in origin, is better? It could be argued that apexogenesis will make the tooth more suitable for restoration, as teeth which have undergone apexification tend to be more fragile and prone to cervical fractures.
Any attempt to undergo biological healing should prove to be more beneficial in the long term. Further research is required into this novel approach to apexogenesis to assess the long-term prognosis of these teeth. Current research on pulp regeneration is growing and provides exciting possibilities for greater biological approaches to endodontics in the future13.
About the authors
Robert Smyth BDS, MFDS RCPSG, MFDS RCSEd graduated from Queen’s University of Belfast in 2012. Following two years working in general practice in Ballyclare and Cookstown, Northern Ireland he took up a core training job at the Edinburgh Dental Institute.
Bob Philpott BDS, MFDS RCSI & RCSEng, MClinDent (UCL), MRD RCSEd Bob Philpott graduated with a BDS from the Cork University Dental School. He subsequently completed a house officer position at the University Hospital of Wales in Cardiff and undertook his specialist training in endodontology at the Eastman Dental Hospital, London, completing his Membership in Restorative Dentistry of the Royal College of Surgeons, Edinburgh.
Bob has specialist registration in both England and Australia, having spent two years in Melbourne working in private practice and at La Trobe University as a clinical supervisor. At the end of 2013, he returned to the UK to take up a position as a locum consultant in endodontics at Glasgow Dental Hospital.
He now works as a senior clinical lecturer/honorary consultant at the Edinburgh Dental Institute and also works in private practice at Edinburgh Dental Specialists.
References
1. American Association of Endodontists. Glossary of endodontic terms, 7th edn. Chicago: American Association of Endodontists; 2003
2. Simon S., Smith A.J. Regenerative Endodontics. Br Dent J. 2014 Mar;216(6):E13
3. Cvek, M., Andreasen, J. O. and Borum, M. K. (2001), Healing of 208 intraalveolar root fractures in patients aged 7–17 years. Dental Traumatology, 17: 53–62.
4. Vier, F. V. and Figueiredo, J. A. P. (2002), Prevalence of different periapical lesions associated with human teeth and their correlation with the presence and extension of apical external root resorption. International Endodontic Journal, 35: 710–719.
5. Kim Y-JA, Chandler NP. Determination of working length for teeth with wide or immature apices: a review. International Endodontic Journal, 46, 483–491, 2013.
6. Marcos-Arenal JL, Rivera EM, Caplan DJ, Trope M (2009) Evaluating the paper point technique for locating the apical foramen after canal preparation. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 108, e101–5.
7. El Ayouti A, Dima E, Löst C (2009) A tactile method for canal length determination in teeth with open apices. International Endodontic Journal 42, 1090–5.
8. Hülsmann, M., Peters, O. A. and Dummer, P. M.H. (2005), Mechanical preparation of root canals: shaping goals, techniques and means. Endodontic Topics, 10: 30–76.
9. Rafter, M. (2005), Apexification: a review. Dental Traumatology, 21: 1–8.
10. Banchs F, Trope M (2004) Revascularisation of immature permanent teeth with apical periodontitis; new treatment protocol? Journal of Endodontics 30, 196–200.
11. Shin SY, Albert JS, Mortman RE (2009) One step pulp revascularization treatment of an immature permanent tooth with chronic apical abscess: a case report. International Endodontic Journal 42, 1118–26.
12. McCabe P. (2014) Revascularization of an immature tooth with apical periodontitis using a single visit protocol: a case report. International Endodontic Journal 47.
13. Simon S., Smith A.J., Lumley P.J. et al. (2012) The pulp healing process: from generation to regeneration. Endodontic Topics 26, 41-56.
Verifiable CPD Questions
Aims and objectives:
- To highlight the aetiological causes for this clinical presentation
- To identify the problems which may arise in endodontically treating these teeth
- To outline technique tips to overcome these issues in practice.
Learning outcomes:
At the end of the article, the reader will:
- Have a better understanding of the anatomy of these cases
- Have improved their troubleshooting in the clinical management of teeth with open apices
- Understand the difficulties that may arise clinically during the root canal preparation and most notably, obturation of these teeth
- Recognise the value of newer materials for obturation
- Have a knowledge of new developments in this area of endodontics.








Comments are closed here.