Implant dentistry in 3D
An overview of the development of 3D digital technology, from imaging to printing and how these advances aid the practice of guided implant surgery
A visitor to the biennial International Dental Show (IDS) held in Cologne in March this year could have been mistaken for thinking that they were attending an engineering trade show rather than a dental event. The number of companies displaying milling machines, 3D printers, CAD-CAM hardware and software reflected the rapid developments in digital dentistry in recent years.
There is no area of dentistry that is not being ‘disrupted’ by the move from traditional analogue to digital practice, and implant dentistry is no exception. Planning software has been available for many years, but the recent addition of two concepts has seen a renewed interest in guided surgery. This article will examine optical scanning and desktop 3D printing in the production of drill guides, that may facilitate accurate surgical technique benefiting both the clinician and patient.
The aim of a detailed pre-surgical assessment is to ensure that the implant is placed in an optimal position so that it may be restored to achieve the desired aesthetic and functional result. Clinical and radiographic examination of the patient is required before implant placement. The assessment should consist of visual examination, palpation of superficial structures and the measurement of gap width, crest width and maxillo-mandibular relationships.
Radiographs are used during implant treatment planning and Cone beam computer tomography (CBCT) is used to view a 3D image of hard tissue. This enables the clinician to measure the height and width of the ridge and assess the quality of the planned implant site and adjacent anatomical structures. While there is still a place for conventional 2D imaging techniques, the use of a CBCT scan is now considered to be standard practice in implant dentistry1,2.
The images from CBCT scans may be imported into many software packages to allow the clinician to plan the implant placement in a virtual environment prior to surgery. Programmes such as Simplant (Dentsply Implants) have had the ability to not just plan implant placement, but to use CAD (computer aided design) output to CAM (computer aided manufacture) to produce drill guides for many years. Thus, it is important to state that neither the use of CBCT or guided surgery is new.
The use of guided surgery has previously been restricted by two factors:
- Inability of CBCT to provide intra-oral soft tissue images
- Cost of drill guide manufacture.
Intra-oral scanning provides detailed surface images of the dental hard and soft tissue. These images may be merged with hard-tissue images from a CBCT scan to provide a 3D view of teeth/bone and of soft issue. As with previous software, CAD planning allows the manufacture of drill guides. The availability of affordable 3D printers now allows the dentist to produce in-house accurate and cost-effective drill guides.
Both intra-oral scanning and 3D printing date back to the 1980s. Nearly 30 years later, both are changing the way we plan implant dentistry.
Optical intra-oral scanner
CEREC 1 was developed by Dr Werner H Mormann and Dr Marco Brandestini at the University of Zurich. Thanks to more powerful (and smaller) computers and the developing application of CAD/CAM systems at the time, their vision resulted in the first of the series of CEREC machines. From its early beginnings, limited to milling ceramic inlays, optical scanning and CAD/CAM manufacture are today at the focus of many developments in restorative and
surgical dentistry.
Optical scanners work by directing a light beam at an object, the light beam is bounced back to the scanner and the image is digitised. A digital image is a series of triangles joined together to make a 3D image – a meshwork of triangles – stored in digital format.
STL (STereoLithography) is the file format of stereolithography CAD software that is widely used for rapid prototyping, 3D printing and computer-aided manufacturing. Images from dental optical scanners may output to STL files (open platform) or a scanner specific file format (closed platform). The two market-leading intra-oral scanners, Trios (3Shape, Denmark) and CEREC (Dentsply Sirona, Germany) have both recently enabled STL file output for their respective scanners. This move to STL open-platform enables dentists and dental labs to make use of the STL files in a wide range of software packages, rather than being restricted to a closed-platform programme.


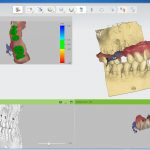
In relation to implant planning software, the STL file is imported and combined with DICOM (Digital Imaging and Communication in Medicine) data from the CBCT scan (Fig 1). Many planning programmes are available – a selection is listed in Table one. A comparison of the strength and weaknesses of each is outwith the scope of this article but, as with any software, one should assess its ease of use, support, cost, open/closed platform.
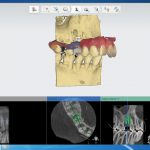
The software allows the dentist to plan the implant position (Fig 2) and then design a drill guide (Fig 3). The design is outputted to an STL file, which can then be sent to a 3D printer either on-site or to a third party e.g. a dental lab.
- Figure 1
- Figure 2
- Figure 3
- Figure 4
- Figure 5
- Figure 6
- Figure 7
- Figure 8
3D printing
Early additive manufacturing equipment and materials were developed in the 1980s. 3D printing, also known as additive manufacturing or rapid prototyping, refers to processes used to create a three-dimensional object in which layers of material are formed under computer control to create an object. 3D printing builds a three-dimensional object from a CAD model by successively adding material layer by layer.
An early use of 3D printing in dentistry was shown in 1984 when a team working on sub-periosteal implants at Loma Linda University in California used 3D printing to produce a mandible from a CT scan3. The printed model of the mandible was then used to manufacture the sub-periosteal implant. The CT scan and 3D print removed the need for a surgical visit to take an impression of
the mandible.
The size and cost of 3D printers has fallen, while the range of 3D printers continues to grow at an astonishing pace. Originally aimed at industrial manufacturers, 3D printers are now available for all, from those aimed at the domestic hobbyist, to small and medium-sized business and large-scale operations.
In recent years, dental applications in desktop 3D printing have rapidly taken off. FormLabs (Massachusetts, US) products have been at the forefront of dental innovation. Aimed at the “prosumer” (production by consumer) market, dentists and dental labs now use the Form 2 (Fig 4) to create surgical guides, study models, bleaching trays, retainers, aligners, and with the imminent launch of FormLab denture resin, it will soon be possible to 3D print dentures. The Form 2 printer has a range of dental resins detailed in Table two.
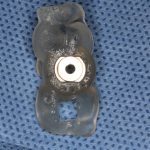
The dental SG resin is an autoclavable, class 1 medical device directive registered biocompatible resin. Dental SG is used for printing surgical guides. It was launched by FormLabs in 2016 and was the first biocompatible resin for desktop 3D printing. Following 3D printing in the Form 2, dental SG is light cured in a light oven (Fig 5) (Brelux Power Unit 2, Bredent GmbH, Germany), the appropriate drill sleeve is selected and fitted for either a pilot of fully guided surgery (Fig 6). The drill guide may then be autoclaved prior to surgery.
Direct printing of surgical guides has traditionally required large-scale 3D printers that are beyond the expense of most dental laboratories and practices. The introduction of dental SG Resin and the Form 2 allows for surgical guide printing in dental practices and smaller dental labs.
Discussion
It has previously been possible to combine intra-oral detail with a CBCT scan without using an optical scanner. This was achieved using a dual scan technique, whereby a CBCT scan of a study model provided surface hard and soft tissue detail that could be merged with a CBCT scan. In edentulous cases where there is no intra oral hard tissue, it is not possible to use optical scans as intra-oral soft tissue cannot be linked to a CBCT scan. In such cases it is still necessary to use a dual scan technique with radiopaque markers in a denture. Thus, merging intra-oral and CBCT scans is restricted to dentate and partially edentulous cases.
The case for the use of drill guides is that they increase the accuracy of implant placement. Many studies have evaluated the accuracy of guided surgery4,5,6. There is a perception from the marketing of guided surgery by implant companies that this technique is easier than non-guided surgery. In many cases this may be correct, but it is essential that anyone undertaking guided surgery has a sound understanding of implant case planning and surgical protocols. The guide does not place the implant, the surgeon places the implant. The surgeon must be familiar with conventional approaches to implant placement and bone generation techniques before embarking on guided surgery.
It is important to state that guided surgery does not mean flapless surgery. 3D printed guides may be used for the following:
- As pilot guides only with an appropriate muco-periosteal flap
- Fully guided with an an appropriate muco-periosteal flap
- Fully guided with a flap-less technique (Fig 7).
The surgical flap (or lack thereof) will be determined by the need for augmentation at the time of surgery. Flap-less surgery should be restricted to cases with ample bone volume and no need for either soft or hard tissue augmentation. Where there is any doubt with regard for the need for augmentation, an appropriately designed flap should be raised. Where suitable, the benefits of flap-less surgery with a drill guide include: reduced surgery time, minimal post operative complications, no sutures.
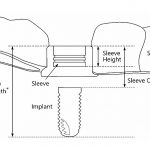
Drill sleeves for pilot guides will be determined by the diameter of the pilot drill, with a range of different sizes that are fitted to the guide following 3D printing. Drill sleeves for fully guided surgery are specific to the implant system being used. The surgeon should have additional training in the use of the guided surgical kit. This differs from the standard surgical kit in that each drill will have a stop to determine the depth of the osteotomy relative to the drill sleeve.
The drill is designed so that there is an offset between the drill sleeve and depth of the planned osteotomy (Fig 8). Inner sleeves or keys are used to match the diameter to the corresponding osteotomy drill (Fig 6). Each step of guided surgery is detailed on a drilling protocol supplied with the treatment plan.
The surgeon placing the dental implant is responsible for the implant placement, not the drill guide. The treatment plan for guided surgery must be approved by the implant dentist prior to 3D printing. When the dental surgeon is the dentist planning the guide, this is straightforward. In situations whereby the CBCT scan/implant planning is referred to a third party, then it is essential that there is effective communication between the parties and that the guided plan is approved by the referring dentist, who is ultimately responsible for the implant placement.
Clinical records including intra-oral images from an optical scanner, CBCT scan, treatment plan and drill guide demonstrate a high standard of planning and record keeping. Such documentation may be of benefit for medico-legal purposes. As with CBCT scans, it may be that this approach will become the gold standard of implant treatment planning and record keeping.
Conclusion
It seems that all of the pieces of the guided surgery jigsaw puzzle have now fallen into place: CBCT, optical scanning, CAD/CAM software and desktop 3D printing. Digital techniques, both hardware and software, are changing the way that dentistry is practised with benefits for both dentists and our patients. Implant companies are promoting guided surgery and it is essential that dentists are trained in such techniques and have a full understanding of the benefits and limitations of guided surgery. At the end of the day, computers and robots don’t place the implants… not yet, at least.
About the authors
Michael Dhesi is a GDP at Clyde Dental Centre. He qualified in 2012 with BDS(Hons) from the University of Glasgow and has subsequently completed MFDS RCPS(Glasg) and an MSc in Advanced General Dental Practice at the University of Birmingham. Michael’s focus is in minimally invasive and adhesive restorative dentistry.
He also has interests in the management of dental anxiety and oral surgery and welcomes referrals in these areas.
Clive Schmulian qualified from Glasgow University in 1993. Throughout his time in general dental practice, he has developed his clinical skills by obtaining a range of postgraduate qualifications, which in turn led him to develop an interest in digital imaging in both surgical and restorative dentistry. He is a director of Clyde Munro.
References
1. Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants. 2014;29 Suppl:55-77.
2. Jacobs R, Quirynen M. Dental cone beam computed tomography: justification for use in planning oral implant placement. Periodontol 2000. 2014 Oct;66(1):203-13.
3. Truitt HP1, James R, Altman A, Boyne P. Use of computer tomography in subperiosteal implant therapy. J Prosthet Dent. 1988 Apr;59(4):474-7.
4. Raico Gallardo, da Silva-Olivio, Mukai, Morimoto, Sesma, Cordaro L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: a systematic review and meta-analysis. Clin Oral Implants Res. 2017 May;28(5):602-612.
5. Ángeles Fernández-Gil, MD/Herminia Serrano Gil, MD/Miguel González Velasco, PhD/José C. Moreno Vázquez, MD, PhD. An In Vitro Model to Evaluate the Accuracy of Guided Implant Placement Based on the Surgeon’s Experience. JOMI. Volume 32, Issue 3 May/June 2017 Pages 515–524.
6. Corina Marilena Cristache, Silviu Gurbanescu. Accuracy Evaluation of a Stereolithographic Surgical Template for Dental Implant Insertion Using 3D Superimposition Protocol. Int J Dent. 2017; 2017.
Verifiable CPD Questions
Aims and objectives
- To provide an overview of the integration of 3D printing in implant planning.
- To discuss the integration of CBCT images and STL files in implant planning.
- To demonstrate the use of in-house 3D printed surgical guides can improve the predictability of treatment outcomes.
Learning outcomes:
At the end of this article, readers will:
- Understand how to integrate 3D printing in implant planning
- Understand the integration of CBCT imaging and STL files in implant planning
- Understand how in-house 3D printed surgical guides can improve the predictability of treatment outcomes.





Comments are closed here.