Endodontic retreatment
Arvind Sharma presents the first in a two-part article looking at a non-surgical root canal retreatment of the mandibular left first premolar (LL4)
A 49-year-old male patient attended for an emergency appointment due to experiencing pain and swelling from a lower left tooth/teeth. He was experiencing pain with biting and pressure. Patient had been experiencing pain from the lower left quadrant for the past few days and the tooth area had now become swollen. He reported no sleep loss or pain with temperatures reported. The quality of pain reported as a dull throbbing pain.
Patient was able to identify tooth LL4 as the source of pain. Analgesics (paracetamol and ibuprofen) had been taken.
Patient had RCT on tooth LL4 while on holiday in Las Vegas, Nevada, US, in 2003. Emergency treatment had been provided by a GDP and definitive RCT completed. A temporary restoration had been placed. On return to Scotland, a composite onlay had been provided as a definitive coronal restoration since the patient reported no pain and was reassured by the Las Vegas dentist that treatment had been completed. The radiograph copy provided by the patient showed a completed root canal treatment on tooth LL4 with all visible canals obturated. Tooth LL4 had been symptom-free until now.
A failed primary root canal treatment. This diagnosis was reached after careful consideration of the clinical signs and symptoms, the special test results and the radiographic information
Arvind Sharma
Previous dental history
The patient is registered with NHS Scotland. He is a regular attender, attending six-monthly examinations and hygienist appointments. He is well-motivated about his dental health.
Previous medical history
No relevant medical history noted. No medication taken. Patient was a smoker (20 per day) up until March 2011.
Social history
Married. Telephone engineer. Non-smoker and moderate alcohol intake.
Examination
Extra-oral
Examination revealed some submandibular swelling on the left mandible. No other significant findings noted.
Intra-oral (Fig 1a-c)
- Soft tissues – Some gingival swelling was palpable buccal to tooth LL4. Oral mucosa, tongue, sublingual tissue and soft/hard palate appeared within normal limits. LL4 was also tender to percussion and appeared to have a small degree of mobility. No lingual swelling was noted.
- Periodontal condition – A Basic Periodontal Examination was recorded as per Table 1.
- Occlusal examination – Angles class I anterior relationship; Class I molar relationship on the left and
a Class I canine relationship on the right. Left and right lateral excursions were canine guided.
Protrusive guidance was provided by palatal surfaces of the maxillary incisors. - Dentition – The dentition present are recorded in Table 2.
The dentition was heavily restored posteriorly on the left and with 1 occlusal restoration present on the right. Upper anterior incisors had porcelain bonded crowns in situ. - Specific examination of the problem site (LL4) – Tooth LL4 was restored with a composite onlay in situ. This was fitted in 2009 and had a good marginal seal and good occlusal relationship with the maxillary teeth. Intercuspal relationship was noted and the buccal cusp was involved in left lateral excursions. There were no isolated periodontal probing defects, no signs of coronal or root fracture and the tooth was TTP.
| 2 1 4 |
| 4 3 3 |
| 7 4 3 2 1 1 2 3 4 5 6 7 |
|---|
| 7 4 3 2 1 1 2 3 4 5 6 7 |
Special investigations
Special investigations were carried out in order to form a provisional and ultimately a definitive diagnosis and to enable the formulation of a definitive treatment plan. The tests performed with results are provided in Table 3 above. The contralateral tooth was used as a control.
Special investigations
| Special test | LL3 | LR4 |
|---|---|---|
| Digital axial/horizontal pressure | Yes | No |
| TTP-axial/horizontal | Axial | No |
| Digital palpation-buccal/lingual | Buccal/lingual | No |
| Endo-Frost | No | Yes |
| EPT | No | Yes |
| Periodontal probing | Within normal limits | Within normal limits |
Radiographic examination
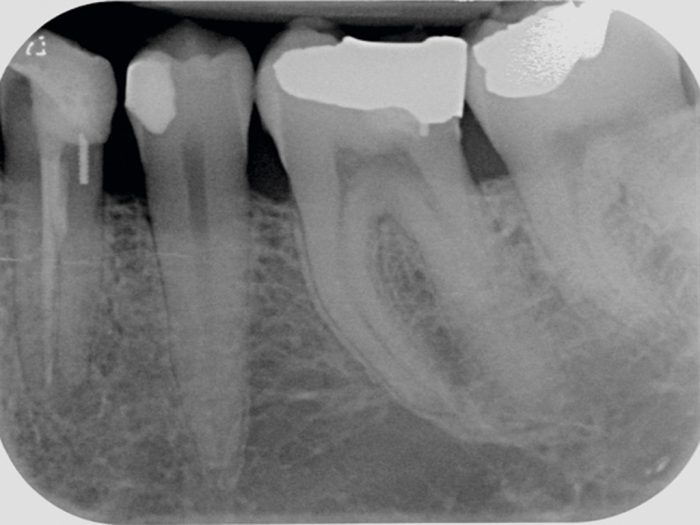
A periapical radiograph (Fig 2) taken at the emergency appointment, revealed a marginally sound coronal restoration. A dentine pin appeared to be present in the distal of the tooth. Some horizontal bone loss was evident at the distal of the tooth. A radio-opaque material was present in the root canal which appeared sub-optimal (non-homogenous obturation) and possibly short of the radiographic apex.
The root appeared wide and a ledge/step was visible mid root with the obturating material. This seemed to suggest two root canals being present with only one obturated. A feint canal root canal space is evident in the distal root. A periapical radiolucency was apparent with some widening of the periodontal ligament space.
The other teeth visible in the radiograph appeared to be clinically sound.
Provisional diagnosis
- Periodontal abscess associated with LL4
- Dental cyst associated with LL4
- Failed primary root canal treatment (apical periodontitis).
Definitive diagnosis
Moderate, non-suppurative, localised, chronic apical periodontitis with a non-obturated root canal. A failed primary root canal treatment. This diagnosis was reached after careful consideration of the clinical signs and symptoms, the special test results and the radiographic information.
Since the special test results showed digital axial/horizontal pressure with axial TTP and tenderness to buccal-lingual pressure, inflammation of the periapical tissues or apical periodontitis, was diagnosed. A dental cyst was considered and it was decided that if definitive treatment was unsuccessful then further tests would be performed to investigate possible cyst formation with associated treatment.
The patient was advised that the reason for treatment was due to bacteria being present in the un-instrumented root canal and quite possibly in the obturated canal also since the obturation appeared suboptimal. Bacterial cause of apical pathology has been shown by Kakehashi et al. 1965 and residual micro-organisms in the root canal system and cementum has been shown by Dalton et al. 1998 and Molander et al. 1999.
Strictly speaking, a definitive diagnosis is only truly possible with a histological analysis of the infected area (Nair et al. 1990 and 1999). However, the resources or facilities for this were not possible.
- Figures 1 a-c: Inra-oral clinical photographs
- Figures 1 a-c: Inra-oral clinical photographs
- Figures 1 a-c: Inra-oral clinical photographs
- Figure 2: LL4 pre-op radiograph
Treatment options
- Reduction of the infection and keep tooth LL4 under observation;
- Reduction of the infection and root canal retreatment of tooth LL4;
- Extraction of tooth LL4 with assessment for prosthetic replacement in 6 months.
Treatment plan
Since the patient was well motivated and wished for a predictable long-term solution he opted for reduction of the infection with root canal retreatment under private contract. He did not wish to keep the tooth under observation since there was a risk of his symptoms returning and he did not wish for extraction of tooth LL4, as this would have functional and aesthetic implications for him.
The treatment procedures with risks were discussed at length. The patient was advised that treatment success would be achieved by removing all of the previous obturation materials, locating the additional canal(s), chemically and mechanically disinfecting the canals and finally obturating the canals and providing a definitive coronal seal.
The patient was given the opportunity to ask questions and these were answered to the patient’s satisfaction. The patient was given a good prognosis upon successful completion of treatment with a success rate approximated at 62-86 per cent based of evidence published by Sjogren et al 1990. The patient was advised that non-surgical root canal retreatment was indicated as a primary treatment option as indicated by Rahbaran et al 2001. Consent was taken and two subsequent appointments made.
Treatment schedule
- Antibiotic prescription to reduce facial swelling
- Oral hygiene advice and instruction plus interdental cleaning demonstration
- Scale and polish
- Restorability assessment and root canal re-treatment of tooth LL4 over two visits
- Definitive composite restoration of access cavity
- Review (one year).
Items 2 and 3 were performed by the practice dental hygienist.
The second part of this article will look at the treatment and case discussion.
References
Dalton BC, Rstavik D, Phillips C, Pettiette M and Trope M, 1998. Bacterial reduction with nickel-titanium rotary instrumentation. Journal of endodontics, 24(11), pp. 763-767.
Kakehashi S, Stanley HR and Fitzgerald RJ, 1965. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surgery, Oral Medicine, Oral Pathology, 20(3), pp. 340-349.
Molander A, Reit C and Dahln G, 1999. The antimicrobial effect of calcium hydroxide in root canals pretreated with 5% iodine potassium iodide. Dental Traumatology, 15(5), pp. 205-209.
Nair PR, Sjgren U, Figdor D and Sundqvist G, 1999. Persistent periapical radiolucencies of root-filled human teeth, failed endodontic treatments, and periapical scars. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 87(5), pp. 617-627.
Nair PR, Sjgren U, Krey G, Kahnberg K and Sundqvist G, 1990. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. Journal of endodontics, 16(12), pp. 580-588.
Verifiable CPD Questions
AIMS and objectives:
- To review clinical history and endodontic diagnosis
- To recognise the importance of preoperative radiographs
- To illustrate to the clinician the complexity of root canal anatomy of mandibular first premolars
- To highlight the benefits of a microscope in endodontics
- To provide the clinician some of the advantages of heated obturation.
Learning outcomes:
- Be aware of the incidence and location of additional canals in mandibular first premolars and be able to assess and diagnose mandibular first premolars which may have two root canals
- Be able to highlight the importance of microscopes in endodontic case management
- Know when to consider making an endodontic referral.





1 Comment
Well Nice Information On The Given Topic, Very Helpful In Every Manner For Us, Will Be Visiting Again For More Useful Info On The Topic